Side Effect Understanding Tool
Understand What "Common" Really Means
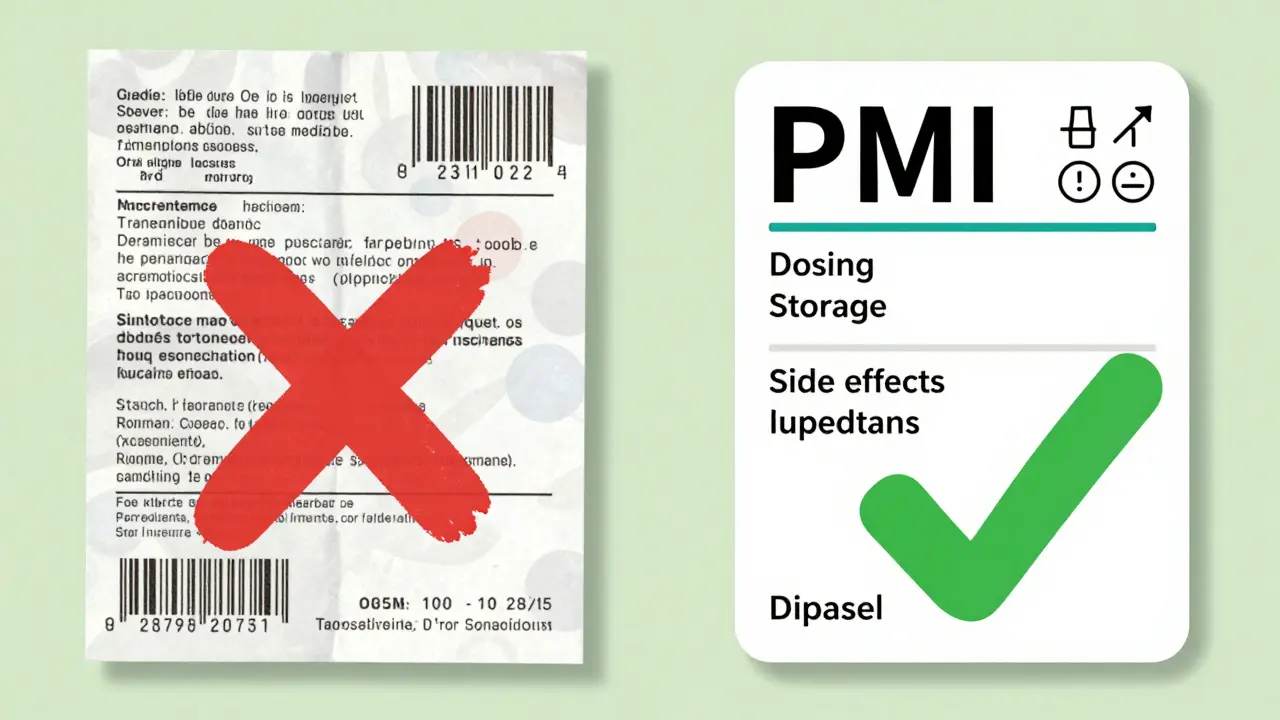
The FDA's new Patient Medication Information (PMI) is designed to help you understand medication side effects better by showing actual percentages instead of vague terms like "common." Enter the percentage of people who experience a side effect to see how it translates to real-world situations.
Example: If 43% of people experience headaches, then out of 100 people taking this drug, approximately 43 would experience this side effect.
Why This Matters
The FDA's new PMI is designed to replace vague terms like "common" with actual percentages, helping you better understand medication risks. For example, the article notes that while current PMI says "Headache is a common side effect," the University of Pittsburgh's version states "43% of people who take this drug get a headache." This clarity helps you make informed decisions about your medication.
The U.S. Food and Drug Administration (FDA) is proposing a major change to how prescription drugs come with patient information - and it could affect every single person who takes a pill, shot, or infusion outside a hospital. Right now, only about 150 out of thousands of prescription drugs come with a Medication Guide. That’s less than 10% of all prescriptions. Starting in 2025, patient medication information (PMI) will be required for every single outpatient prescription drug in the U.S.
What Exactly Is the PMI?
The new Patient Medication Information (PMI) is a single-page, standardized handout that every pharmacy will hand out with your prescription. It’s not a reprint of the doctor’s notes or a pharmacy label. It’s a clean, simple, FDA-approved document designed to tell you what you absolutely need to know to use your medicine safely.It starts with one clear line: “Use exactly as prescribed.” No fluff. No marketing. Just the facts. Then it breaks down:
- How to take it - morning or night? With food or on an empty stomach?
- How to store it - fridge? Room temperature? Keep away from kids?
- What to do if you miss a dose
- How to safely dispose of leftover pills
- Warning signs - what side effects mean you need to call your doctor right away
- Common side effects - like headaches, nausea, or dizziness
The layout is tested with real patients. The font is 12-point. The language is plain. No jargon. No fine print. The goal? To help the 80 million U.S. adults with low health literacy understand their meds better.
Why This Change Is Happening
Right now, medication errors cause about 1.3 million injuries and 7,000 deaths every year in the U.S. - according to the Institute of Medicine. Many of these happen because patients don’t understand how to take their drugs.Pharmacy labels vary wildly. One pharmacy might list your name and insurance info in giant letters. Another might bury the dosage instructions under a barcode. Patients get confused. They skip doses. They double up. They take pills with grapefruit juice because they didn’t know it could be dangerous.
The current Medication Guides? They’re only required for high-risk drugs - opioids, blood thinners, certain cancer treatments. But what about the 90% of other prescriptions? Antibiotics? Blood pressure pills? Antidepressants? You get a tiny slip of paper with no clear instructions. The PMI fixes that.
Studies show patients who get clear, consistent instructions are 30% more likely to take their meds correctly. That’s not just about safety - it’s about effectiveness. If you don’t take your statin every day, your heart attack risk doesn’t go down. If you don’t finish your antibiotic, you risk creating superbugs.
What’s Different From Today’s Medication Guides
The big difference? Scope. Right now, Medication Guides are the exception. PMI will be the rule.Current Medication Guides:
- Only for about 150 drugs
- Focus on serious risks - like suicidal thoughts or bleeding
- Format varies by manufacturer
- Often long, dense, and hard to read
New PMI:
- Required for ALL outpatient prescription drugs
- Standardized format - same layout, same order, same language
- One page only - no more than 250 words
- Designed for quick understanding - tested with patients
- Includes directions, storage, disposal, and common side effects - not just rare dangers
That means if you’re on a generic blood pressure pill, an antihistamine, or a diabetes med - you’ll get the same clear, consistent info as someone on a high-risk drug. No more guessing.
Electronic Options and Accessibility
You won’t have to take paper if you don’t want it. The FDA is requiring electronic versions too - through pharmacy apps, patient portals, or email. But here’s the catch: it must be accessible.That means:
- Text must be readable by screen readers
- Color contrast must meet Section 508 standards
- Files must be downloadable and printable
This isn’t just about convenience. It’s about equity. Older adults, people with visual impairments, and those without smartphones still need access. Pharmacies will still offer paper copies. The electronic option is just that - an option.
What’s Missing? The Criticisms
The PMI is a big step forward - but it’s not perfect. Researchers at the University of Pittsburgh tested their own version called “Decision Critical PMI.” They found patients wanted more.Right now, the FDA’s PMI says: “Headache is a common side effect.”
The Pittsburgh version says: “43% of people who take this drug get a headache.”
That difference matters. “Common” means different things to different people. Is it 1 in 10? 1 in 2? Knowing the actual percentage helps you decide if it’s worth the risk.
Another gap? Benefits. The PMI doesn’t say how well the drug works. If you’re taking a cholesterol pill, you won’t know if it lowers your LDL by 20% or 40%. That’s information your doctor should give you - but if you’re reading the PMI to make a decision, you’re left guessing.
The FDA says this is intentional. They want the PMI to be short, scannable, and focused on safety. They assume your doctor already explained the benefits. But not everyone has that conversation. And if you’re reading the PMI because you’re unsure - you’re missing key context.

Who’s Paying for This?
The cost won’t come out of your pocket - but it’s real. Industry analysts estimate $1.2 billion in total costs over five years.- Pharmaceutical companies (65%) - writing, testing, and submitting PMIs for every drug they make
- Pharmacies (25%) - updating systems, training staff, printing, distributing
- Doctors and clinics (10%) - updating patient education materials
Smaller pharmacies are worried. About 15% of independent pharmacies say they might struggle with the time and cost. Each prescription will take 30 to 60 seconds longer to fill at first. Pharmacists will need 2 to 4 hours of training. Annual refreshers? One hour.
The FDA says they’ll help. They’re creating templates. They’re building a review team to handle over 10,000 PMI submissions a year. But for small manufacturers and rural pharmacies, this is still a heavy lift.
When Will This Happen?
The proposal was published in May 2023. The public comment period closed in November 2023. The FDA is reviewing over 1,200 comments from patients, doctors, drugmakers, and pharmacists.Final rule expected: Q2 2024
Implementation begins: 2025
Big drugmakers: 24 months to comply
Small manufacturers: 36 months to comply
By the end of 2025, every prescription you pick up - whether it’s insulin, ibuprofen, or a new antidepressant - will come with the same clear, simple, one-page PMI.
What This Means for You
If you take prescription drugs, this change is personal. You’ll get better information. Fewer mistakes. More confidence.Here’s what to do now:
- Ask your pharmacist: “Will I get the new PMI when this rule starts?”
- Read the new PMI carefully - even if you’ve taken the drug before. Things change.
- Don’t ignore the side effect list. If you feel something new, write it down.
- If you’re unsure what a term means, ask. “What does ‘common’ mean here?”
- Keep your PMI. Don’t throw it away. Use it as a reference.
This isn’t just a paperwork update. It’s a shift in how medicine is communicated. The FDA is finally putting the patient’s understanding first - not the manufacturer’s marketing, not the pharmacy’s billing system, not the doctor’s rushed instructions.
It’s not perfect. But it’s a start. And for millions of people who’ve been confused by their prescriptions - it’s long overdue.


Chris Buchanan
December 22, 2025 AT 21:49This is finally happening?? I’ve been waiting for this since my grandma mixed up her blood pressure pills with her diabetes meds and ended up in the ER. One page? Clean font? No tiny print? I’ll take it. Even if it’s just a step, it’s a step in the right direction. My mom’s pharmacy still prints labels in Comic Sans. No joke.
Wilton Holliday
December 23, 2025 AT 10:04Love this. 🙌 I work in a clinic and I see patients stare at their pill bottles like they’re decoding alien hieroglyphs. One guy asked me if ‘take with food’ meant he could eat a whole pizza with his antibiotic. This PMI could save lives. Seriously. And yes, the 43% stat thing? That’s the next upgrade. But baby steps, right?
Raja P
December 23, 2025 AT 19:40Not bad. In India, we don’t even get labels in our language half the time. But if this works in the US, maybe it’ll push pharma companies to do better globally. Simple language = less death. That’s not politics, that’s basic human decency. Hope it sticks.
Joseph Manuel
December 24, 2025 AT 23:41The FDA’s approach is fundamentally flawed. Standardizing content ignores pharmacokinetic variability across populations. The one-page constraint forces dangerous oversimplification. For example, ‘common side effect’ is statistically meaningless without context. Furthermore, the cost-benefit analysis is skewed - $1.2B over five years for marginal compliance gains. This is regulatory theater dressed as patient safety.
Harsh Khandelwal
December 25, 2025 AT 07:00Let me guess - Big Pharma paid the FDA to make this so they can charge more later. You think they’re doing this for you? Nah. They’re just making sure you don’t sue them when you die from the ‘common’ side effect they buried in paragraph 3. And don’t get me started on the ‘electronic option’ - they’re pushing you to sign up for their app so they can track your meds. Next thing you know, your insurance company gets notified if you skip your antidepressants. 😏
Andy Grace
December 26, 2025 AT 14:21It’s about time. I’ve had patients cry because they didn’t know they couldn’t drink alcohol with their antibiotics. Or that grapefruit juice could kill them. The PMI won’t fix everything, but it gives people a fighting chance. I’m just glad they’re finally listening to what patients actually need - not what the lawyers think they should say.
Delilah Rose
December 28, 2025 AT 11:54I just want to say, as someone who’s been on six different medications in the last three years, I’ve had to call my pharmacist at midnight because the label said ‘take once daily’ but the doctor said ‘take at bedtime’ and the pharmacy sticker said ‘take with food’ but the guide said ‘take on empty stomach’ and I just sat there holding the bottle like a confused child wondering if I was going to die because I took it wrong - and this? This right here? This is the kind of thing that makes you believe in humanity again. Not because it’s perfect, but because someone finally thought, ‘Wait, maybe the person taking this doesn’t have a pharmacy degree.’ And that’s… honestly, kind of beautiful.
Spencer Garcia
December 30, 2025 AT 00:21Good move. Simple, clear, consistent. The 30% adherence boost is real. Pharmacies will adapt. Patients will thank you. No drama needed.
Abby Polhill
December 31, 2025 AT 16:49So the PMI is basically a HIPAA-compliant, FDA-approved, patient-centric, low-literacy-optimized, accessibility-forward, non-commercialized, standardized medication risk disclosure framework. It’s not just a handout - it’s a paradigm shift in pharmacovigilance communication architecture. I mean, we’re talking about closing the knowledge gap between prescriber intent and patient execution. That’s… kinda wild. And also, I’m low-key impressed.
Bret Freeman
January 2, 2026 AT 04:21They’re forcing this on us. Every single pill. Every. Single. One. They’re turning pharmacies into government pamphlet distribution centers. Next thing you know, they’ll make you sign a waiver before you can buy Tylenol. And don’t even get me started on the ‘electronic option’ - they’re tracking you. They’re watching you. They’re building a database of your health habits. And you’re all clapping like this is a gift? Wake up. This isn’t safety. This is control. And it’s coming for your vitamins next.