Anticoagulant Timing Calculator
Calculate Safe Anticoagulant Timing
Enter your medication and procedure details to determine safe timing windows for stopping and restarting anticoagulants according to ASRA guidelines.
Medication Type
Additional Details
Getting an epidural or spinal injection while on blood thinners sounds simple-until something goes wrong. For millions of people taking anticoagulants for atrial fibrillation, deep vein thrombosis, or after joint replacement, these procedures are routine. But beneath the surface of routine care lies a rare, silent threat: spinal epidural hematoma. It’s not common, but when it happens, it can change your life forever.
What Exactly Is a Spinal Epidural Hematoma?
A spinal epidural hematoma (SEH) is a collection of blood that forms between the spinal cord’s protective layer (the dura) and the spine’s inner wall. Even a tiny amount-just 1 to 2 milliliters-can squeeze the spinal cord because the space around it is so tight. This pressure cuts off nerve signals, leading to sudden pain, weakness, or even paralysis. It doesn’t happen often. Studies show the overall risk is about 1 in 150,000 for a simple epidural. But when you’re on blood thinners, that risk jumps. For people on therapeutic doses of low molecular weight heparin (like Lovenox), the risk can be 4.3 times higher. And if you’ve had multiple needle attempts or a traumatic puncture, the chance skyrockets even more.Who’s at the Highest Risk?
Not everyone on blood thinners is equally at risk. Certain factors stack the odds:- Medication type: Warfarin with an INR above 1.4 increases risk by 8.7 times. Therapeutic-dose LMWH carries a 0.31% risk if given less than 8 hours before the procedure. DOACs like rivaroxaban and apixaban have lower but still present risks if timing isn’t perfect.
- Renal function: If your kidneys aren’t clearing the drug properly (CrCl under 30 mL/min), your risk nearly doubles.
- Age: People over 70 have 3.7 times higher risk.
- Procedure type: A single epidural shot for pain is low risk. But placing a catheter, doing a spinal fusion, or inserting a stimulator increases the chance of bleeding significantly.
- Other factors: Low hemoglobin, heavy blood loss during surgery, or spinal stenosis all add up.
How Timing Makes All the Difference
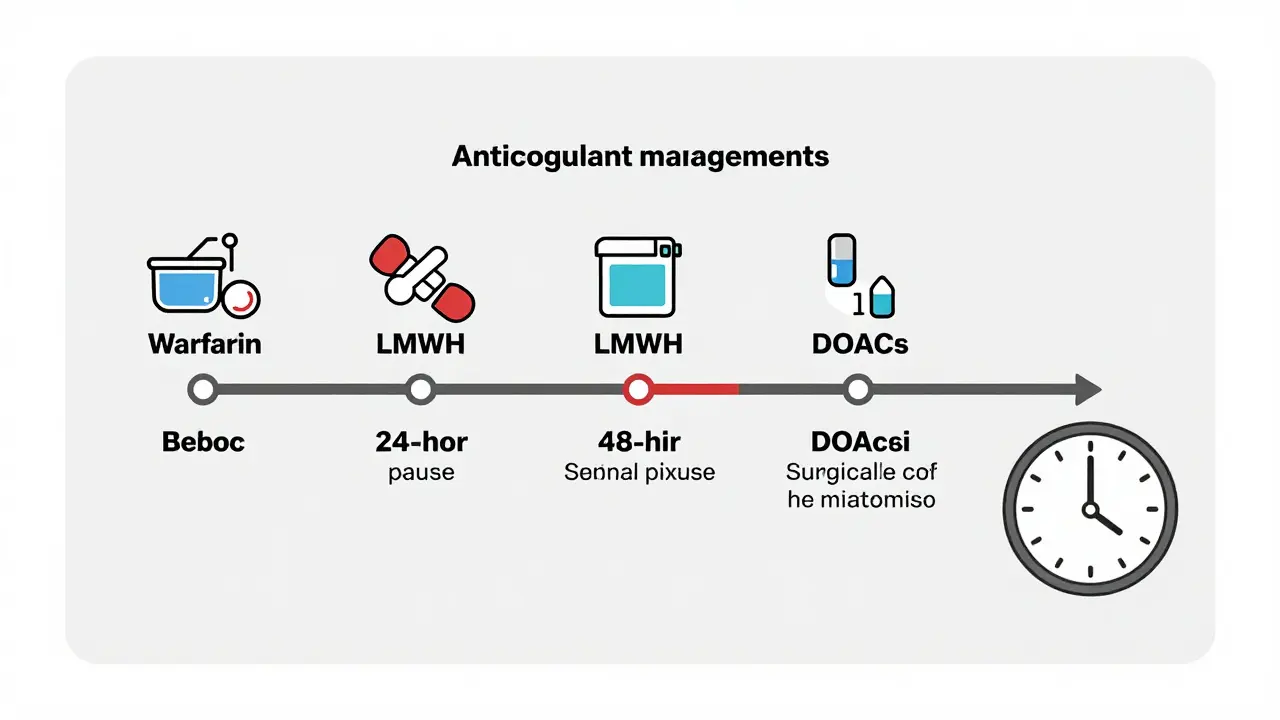
Timing isn’t just important-it’s life-or-death. The guidelines from the American Society of Regional Anesthesia and Pain Medicine (ASRA) are clear, but they’re also complex.- Warfarin: Check your INR within 24 hours before the procedure. It must be under 1.4. You can restart 4 hours after a single shot, 6 hours after a catheter.
- LMWH (Lovenox, Fragmin): Wait 10-12 hours after the last prophylactic dose. For therapeutic doses, wait 24 hours. Restart 2 hours after a single injection, 4 hours after a catheter.
- DOACs (Xarelto, Eliquis, Pradaxa): Stop 48 hours before if your kidneys are normal. If your kidney function is impaired, wait 72 hours. Never skip this window.
What Happens If a Hematoma Forms?
Symptoms come fast. You might feel:- Sharp, midline back pain (93% of cases)
- Numbness or tingling in your legs or groin (89%)
- Weakness or inability to move your legs (76%)
- Loss of bladder or bowel control (34%)
What About Aspirin and Antiplatelets?
This is where things get messy. Some doctors say aspirin is safe. Others disagree. Studies show that single-dose aspirin carries almost no risk-only 0.03% in one study of over 1,200 patients. But dual antiplatelet therapy (like aspirin + clopidogrel) increases risk 3.8 times. If you’re on both after a stent or heart attack, stopping them too early can cause a heart attack or stroke. But keeping them on can cause a spinal bleed. There’s no perfect answer. Most guidelines suggest stopping clopidogrel, prasugrel, or ticagrelor 5-7 days before surgery. But if your heart condition is unstable, your doctor might choose to proceed anyway-knowing the risk.The Cost of a Mistake
The financial toll of a spinal hematoma is staggering. One study found the average cost per case is $287,450. That includes:- $182,600 for initial hospitalization
- $78,300 for rehabilitation
- $26,550 for long-term care if paralysis occurs

New Tools and Changing Guidelines
The field is evolving. In 2023, the FDA mandated a Risk Evaluation and Mitigation Strategy (REMS) for all anticoagulants. That means prescribers must complete training on neuraxial risks before writing prescriptions. New tools are also emerging. Mobile apps like “Neuraxial Anticoag” have been downloaded over 12,000 times. But a 2021 study found 17% of them had outdated info. Always double-check with the latest ASRA guidelines. Upcoming research may change things again. A 2022 study found that a blood marker called GFAP, if above 0.72 ng/mL within 2 hours after a procedure, is 94% accurate at predicting a developing hematoma. That could mean earlier detection-and faster intervention.What Should You Do?
If you’re scheduled for an epidural, spinal, or even a lumbar puncture:- Know exactly what blood thinner you’re on and your dose.
- Tell your anesthesiologist and surgeon-don’t assume they’ll check your chart.
- Ask: “What’s the plan for stopping and restarting my medication?”
- Get your INR or kidney function tested if required.
- Don’t take aspirin or NSAIDs the day before unless cleared.
- After the procedure, watch for back pain, numbness, or trouble peeing. If you feel anything unusual, say something immediately.
Final Thoughts
Spinal procedures on anticoagulants aren’t dangerous if handled correctly. But they’re not harmless either. The data is clear: timing, communication, and vigilance save nerves-and lives. The risk isn’t in taking blood thinners. It’s in not knowing how to manage them around procedures. You’re not just a patient-you’re your own best advocate. Ask questions. Demand clarity. And never assume someone else has checked the details.Can I still get an epidural if I’m on warfarin?
Yes, but only if your INR is below 1.4, checked within 24 hours before the procedure. If it’s higher, you’ll need to stop warfarin and possibly take vitamin K or fresh frozen plasma to reverse it. Never proceed without confirming your INR level.
Is it safe to take aspirin before a spinal injection?
For most people, yes. Single-dose aspirin carries a risk of less than 0.03% in large studies. But if you’re on dual antiplatelet therapy (like aspirin plus clopidogrel), you should stop clopidogrel 5-7 days before the procedure. Always confirm with your doctor.
How soon after the procedure can I restart my blood thinner?
It depends on the drug and type of procedure. For warfarin, restart 4 hours after a single shot or 6 hours after a catheter. For LMWH, wait 2 hours after a single injection or 4 hours after a catheter. DOACs like rivaroxaban or apixaban should be restarted 24-48 hours after, depending on kidney function and procedure risk.
What are the first signs of a spinal hematoma?
The earliest signs are sudden, severe back pain, followed by numbness or weakness in the legs, difficulty urinating, or loss of bowel control. These usually appear within 12 hours. If you notice any of these, tell your medical team immediately-every minute counts.
Do all blood thinners carry the same risk?
No. Warfarin carries higher risk if INR is above 1.4. Therapeutic-dose LMWH has a higher risk than prophylactic doses. DOACs like apixaban have slightly lower risk than rivaroxaban, but timing is still critical. Thrombolytics like tPA are the highest risk and should be avoided entirely for 10 days before neuraxial procedures.
Can a spinal hematoma be treated without surgery?
In very rare cases with mild symptoms and slow progression, doctors may monitor closely and reverse anticoagulation. But for most cases, especially with neurological symptoms, emergency surgery to remove the blood clot is the only way to prevent permanent damage. Waiting increases the chance of lifelong paralysis.
Why do some people get hematomas even when their INR is normal?
Because INR only measures warfarin’s effect. Other factors matter: kidney function, multiple needle passes, traumatic puncture, or even anatomical issues like spinal stenosis. Some people have underlying clotting disorders not caught by standard tests. Timing errors or undocumented doses also play a role.


Katie Schoen
January 5, 2026 AT 02:00Also, why is it that the only time doctors remember to read the guidelines is when someone’s legs stop working?
Jeane Hendrix
January 5, 2026 AT 08:36Rachel Wermager
January 6, 2026 AT 07:03Molly McLane
January 6, 2026 AT 18:53It’s not the meds. It’s the silence.
Ryan Barr
January 8, 2026 AT 17:52Stuart Shield
January 9, 2026 AT 02:56Maybe we need a simple one-pager handed out with the consent form. Not a 20-page PDF no one reads.
Lily Lilyy
January 10, 2026 AT 04:37Let’s make sure no one else has to lose their mobility because of a missed detail.
Leonard Shit
January 12, 2026 AT 01:41Harshit Kansal
January 13, 2026 AT 07:12Brian Anaz
January 14, 2026 AT 00:41Saylor Frye
January 15, 2026 AT 05:41Kiran Plaha
January 15, 2026 AT 16:38Amy Le
January 15, 2026 AT 21:16Indra Triawan
January 17, 2026 AT 03:19Tom Swinton
January 17, 2026 AT 18:51