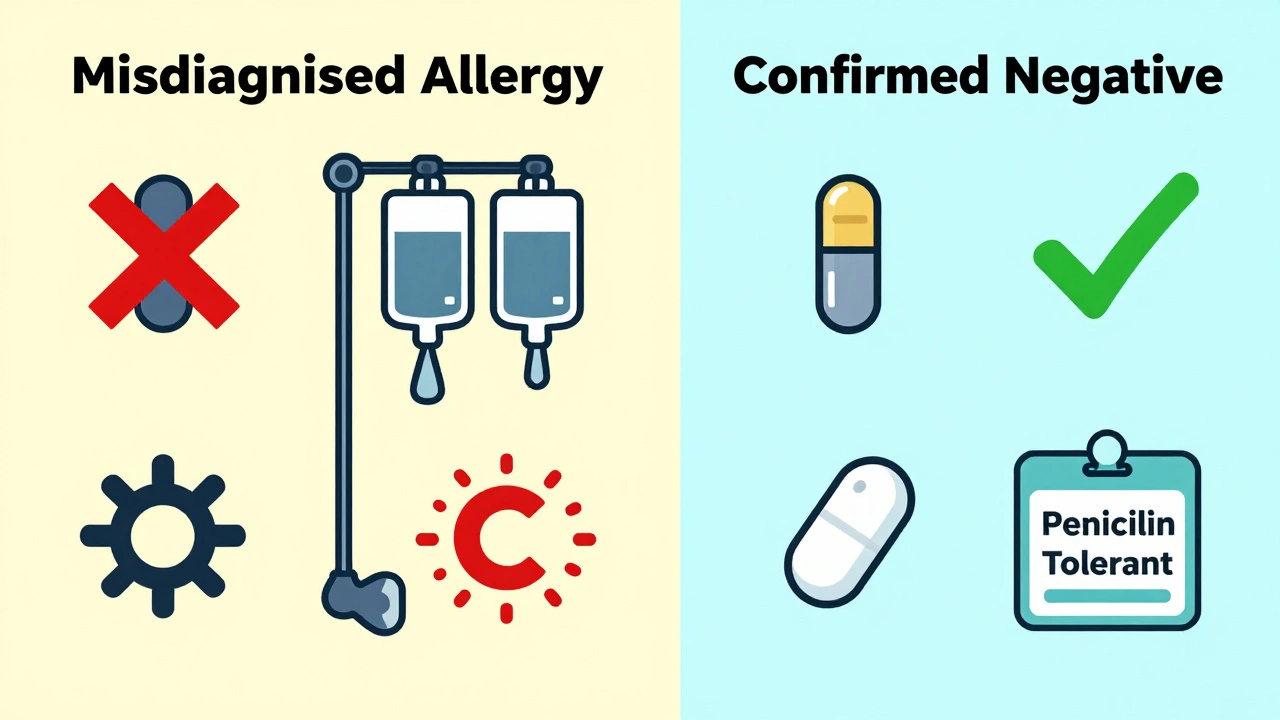
Many people believe they’re allergic to drugs like penicillin-maybe because they got a rash as a kid, or a doctor said so years ago. But here’s the surprising truth: 9 out of 10 people who think they’re allergic to penicillin aren’t. They just had a side effect, a virus, or a reaction that wasn’t an allergy at all. And because of that mislabel, they’re often given stronger, more expensive, and riskier antibiotics instead. That’s where drug allergy skin testing comes in.
What Is Drug Allergy Skin Testing?
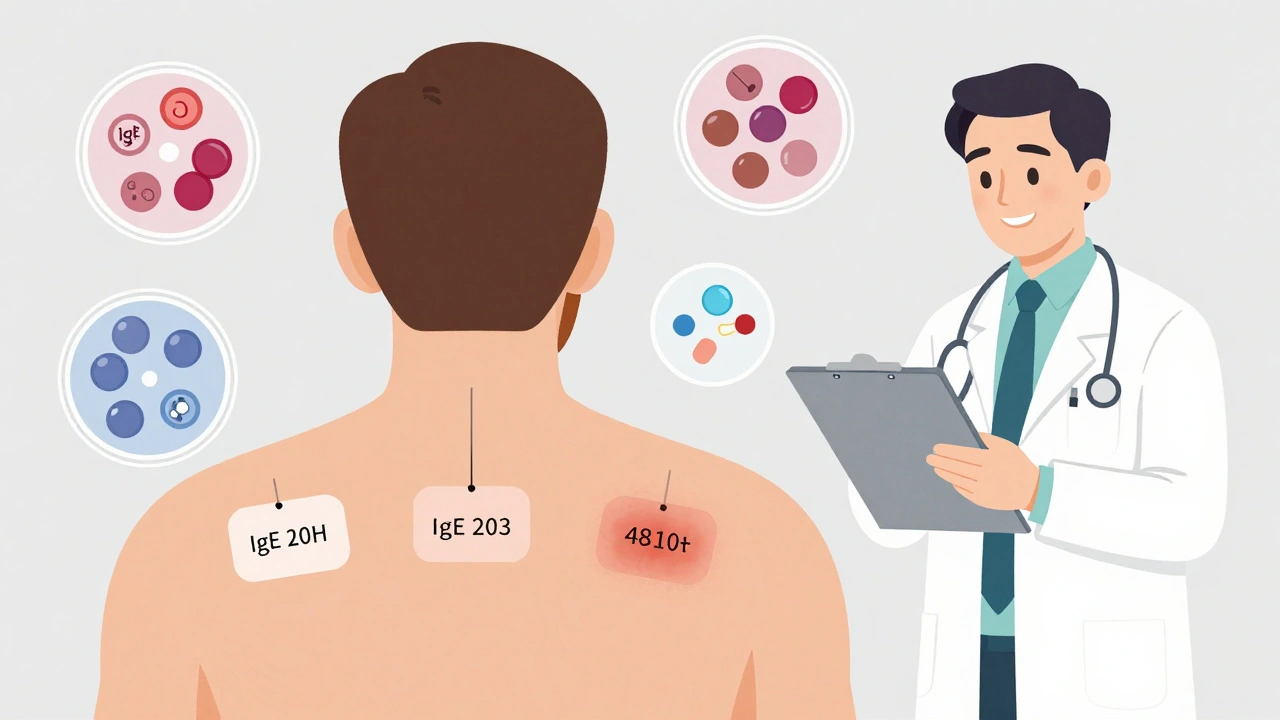
Drug allergy skin testing is a safe, quick way to find out if your body truly reacts to a specific medication. It’s not about guessing. It’s about science. The test looks for IgE antibodies-the same ones that cause hay fever or peanut allergies-but in response to drugs like penicillin, cephalosporins, or even certain painkillers.
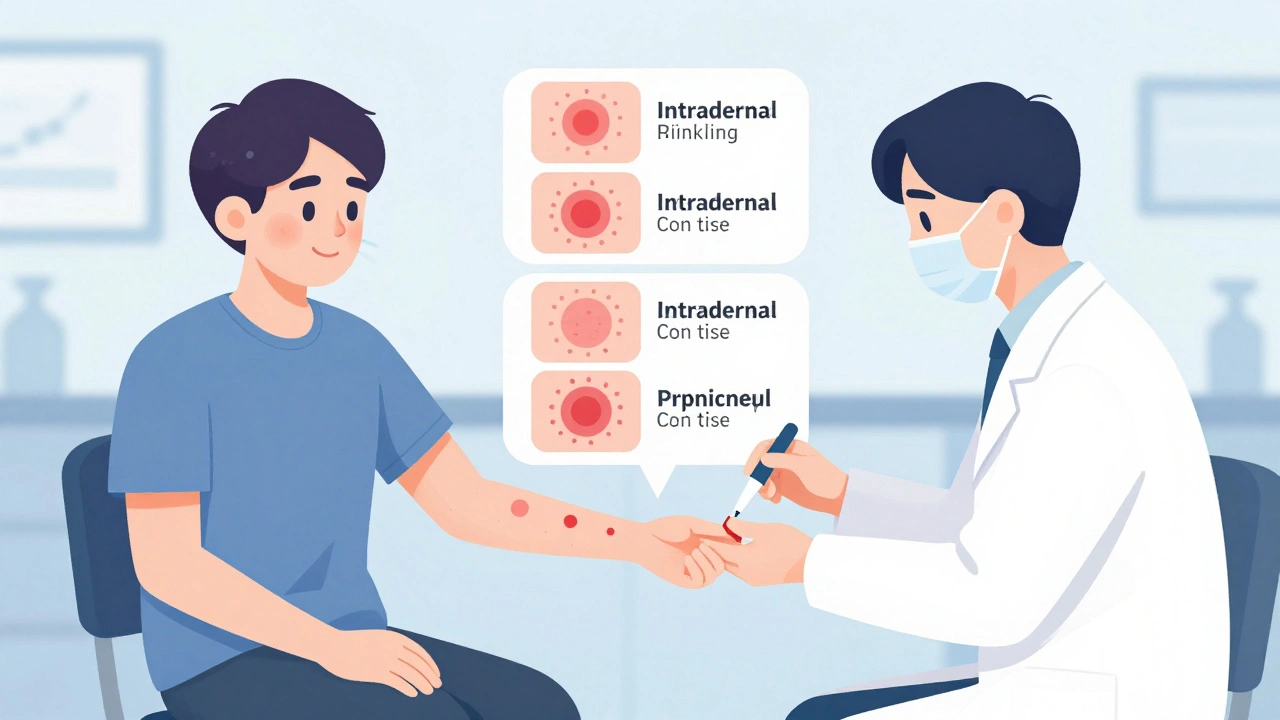
There are three main types of skin tests used for drugs:
- Skin prick test (SPT): A tiny drop of the drug solution is placed on your skin, then the surface is gently pricked with a small needle. It feels like a light mosquito bite.
- Intradermal test (IDT): A small amount of the drug is injected just under the skin with a thin needle, creating a tiny bubble. This is more sensitive and used if the prick test is negative but suspicion remains.
- Patch test: A patch containing the drug is taped to your back for 48 hours. This is used for delayed reactions, like rashes that appear days after taking a pill.
These tests are never done during an active reaction. They’re done when you’re healthy, so doctors can get a clean reading. And they’re always done with controls: one spot gets histamine (to make sure your skin reacts), and another gets saline (to make sure it’s not just irritated by the needle).
How Accurate Is It?
Accuracy depends on the drug. For penicillin, skin testing is one of the most reliable tools in medicine. If both the skin prick and intradermal tests are negative, there’s a 95% to 99% chance you’re not allergic. That means you can safely take penicillin or amoxicillin in the future-no need to avoid it or switch to broader antibiotics.
But it’s not perfect for every drug. For cephalosporins or NSAIDs like ibuprofen, the tests are less reliable. A negative result doesn’t rule out allergy completely. That’s why doctors sometimes follow up with a drug challenge-giving you a small, controlled dose under supervision-to confirm safety.
Why does this matter? Because avoiding penicillin unnecessarily leads to more use of vancomycin, fluoroquinolones, or carbapenems. These drugs are more expensive, can cause C. diff infections, and contribute to antibiotic resistance. Hospitals that offer routine penicillin allergy testing have seen up to a 30% drop in broad-spectrum antibiotic use.
What Happens During the Test?
You’ll sit in a clinic or hospital allergy unit. Your arms or back will be cleaned, and a permanent marker will be used to mark spots-each one at least 2.5 cm apart, away from skin folds like your elbow or wrist.
The skin prick test comes first. The allergist places drops of the drug solution (diluted in saline) on your skin, then lightly pricks the surface. You’ll feel a tiny pinch. No bleeding. No pain. After 15 to 20 minutes, they check for redness, swelling, or itching. A positive reaction looks like a raised, itchy bump-like a mosquito bite that got bigger.
If the prick test is negative, they move to the intradermal test. A small syringe injects just 0.02 to 0.05 milliliters under the skin. You might feel a brief sting. Again, you wait 15 to 20 minutes. A positive result means the bump grew by at least 3 mm compared to the saline spot.
The whole process takes about 45 to 60 minutes. You’ll be monitored the whole time. Staff are trained to handle rare reactions. In fact, systemic reactions during testing are extremely rare-less than 1% of cases. The drug stays in the top layer of your skin. It doesn’t enter your bloodstream in large amounts.
What Should You Do Before the Test?
Preparation is key. If you take antihistamines-like cetirizine, loratadine, or diphenhydramine-you must stop them 5 to 7 days before the test. These drugs block allergic reactions and can make the test falsely negative. That’s why some patients get frustrated: they show up, the test is inconclusive, and they have to reschedule.
Also, avoid any other medications that might interfere unless your doctor says it’s safe. Don’t stop heart meds, blood pressure pills, or asthma inhalers without talking to your doctor first. Only antihistamines and some depression or sleep meds need to be paused.
Wear a short-sleeve shirt. You’ll need access to your arms or back. And don’t apply lotions or creams to the test area that day.
What Does a Positive Result Mean?
A positive skin test means your immune system recognized the drug as a threat. It doesn’t mean you’ll definitely have a bad reaction if you take it again-but it does mean you’re at higher risk. You’ll be advised to avoid that drug and any closely related ones.
For example, if you’re allergic to penicillin, you’ll likely avoid amoxicillin, ampicillin, and other penicillin-based antibiotics. Your doctor will choose alternatives like azithromycin or clindamycin.
But here’s the good part: even if you test positive, you might still be able to take the drug later through a process called desensitization. This is done in a hospital under close watch, slowly building tolerance over hours. It’s not for everyone-but it’s an option for people who need a specific antibiotic for a serious infection.
What About False Negatives?
Yes, they happen. Especially with drugs that don’t have standardized test solutions. For example, testing for sulfa drugs, vancomycin, or ciprofloxacin is harder because reliable reagents aren’t always available. In rare cases, someone tests negative and still has a severe reaction later.
That’s why doctors don’t rely on skin tests alone. They combine them with your medical history. Did you have hives and swelling within an hour after taking the drug? That’s a red flag. Did you get a rash two weeks later? That’s probably not IgE-mediated and might need a patch test instead.
A 2022 case in Medscape showed a patient with negative skin tests to cephalosporins who later went into anaphylaxis during treatment. It’s rare-but it reminds us that testing isn’t magic. It’s a tool. And it works best when used with clinical judgment.
Who Should Get Tested?
If you’ve ever had any of these after taking a drug:
- Hives or swelling (face, lips, tongue)
- Difficulty breathing or wheezing
- Dizziness or fainting
- Severe rash within hours
Then you should consider testing. Especially if you’ve been told you’re allergic to penicillin. That’s the most common mislabeling. Even if it happened decades ago, it’s worth rechecking. Your body can change. Your needs can change.
Also, if you’re facing surgery or a serious infection and your doctor says you can’t use certain antibiotics because of a reported allergy-ask if skin testing is an option. It could open up better, safer, cheaper treatment paths.
Is It Safe?
Yes. Skin testing is one of the safest allergy procedures available. The amount of drug used is tiny-micrograms, not milligrams. It’s not enough to trigger a full-body reaction in most people. The biggest risk is local itching or redness at the test site, which fades within hours.
Clincs always have emergency equipment on hand: epinephrine, oxygen, IV fluids. Staff are trained in anaphylaxis management. You’ll be watched for at least 30 minutes after the last test. Most people leave the same day with no issues.
And if you’re nervous? You’re not alone. Many patients say the anticipation is worse than the test. One Reddit user wrote: “The prick test felt like tiny mosquito bites. The intradermal stung for a few minutes-but knowing it was helping me avoid unnecessary antibiotics made it worth it.”
What Happens After the Test?
Your results are explained right away. If negative, you’ll likely get a letter or card confirming you’re not allergic. Some hospitals give you a medical alert bracelet that says “Penicillin Tolerant” instead of “Penicillin Allergic.”
If positive, you’ll get a list of drugs to avoid and alternatives to use. You might also be referred to an allergist for long-term management.
And here’s the big win: if you’re cleared, you can stop avoiding penicillin-like drugs. That means fewer side effects, lower costs, and better outcomes. Hospitals with formal allergy delabeling programs have seen 22% fewer cases of C. diff infection-a serious gut infection linked to overuse of broad-spectrum antibiotics.
Where Can You Get Tested?
Not every clinic offers it. You need an allergist or immunologist trained in drug allergy testing. In Australia, most major hospitals and private allergy practices have the capability. Ask your GP for a referral. If you’ve had a serious reaction in the past, you’re a good candidate.
Insurance usually covers it if it’s medically necessary. In the U.S., Medicare and most private plans pay for it. In Australia, Medicare rebates apply for specialist allergy consultations. Check with your provider.
And if your doctor says, “We don’t do that here”-ask why. It’s not because it’s risky. It’s often because they’re not trained in it. But that’s changing. More hospitals are adding allergy services because the benefits are clear.
Final Thoughts
Drug allergies are real. But so are misdiagnoses. Skin testing is the best way to know for sure. It’s quick, safe, and can change your medical future. If you’ve been told you’re allergic to a common antibiotic, don’t just accept it. Ask: “Can I be tested?”
You might find out you’ve been avoiding safe, effective drugs for years. And that’s not just about convenience. It’s about better health, fewer side effects, and smarter use of antibiotics-for you, and for everyone else.

Kumar Shubhranshu
December 7, 2025 AT 03:54Mayur Panchamia
December 8, 2025 AT 17:00Karen Mitchell
December 9, 2025 AT 21:42Geraldine Trainer-Cooper
December 11, 2025 AT 14:21Nava Jothy
December 12, 2025 AT 19:44Kenny Pakade
December 13, 2025 AT 21:00brenda olvera
December 14, 2025 AT 09:13Myles White
December 14, 2025 AT 14:14olive ashley
December 15, 2025 AT 08:06Ibrahim Yakubu
December 16, 2025 AT 13:14Brooke Evers
December 17, 2025 AT 20:45Chris Park
December 18, 2025 AT 14:28Saketh Sai Rachapudi
December 20, 2025 AT 09:57joanne humphreys
December 21, 2025 AT 01:34Myles White
December 23, 2025 AT 00:48