Why Diabetic Foot Care Isn’t Optional
One in four people with diabetes will develop a foot ulcer in their lifetime. That’s not a distant possibility-it’s a real, avoidable risk. And once an ulcer forms, the chance of amputation jumps dramatically. The good news? Most of these ulcers start with something small: a blister, a cut, or even just a bit of redness. If you catch it early, you can stop it before it becomes a crisis.
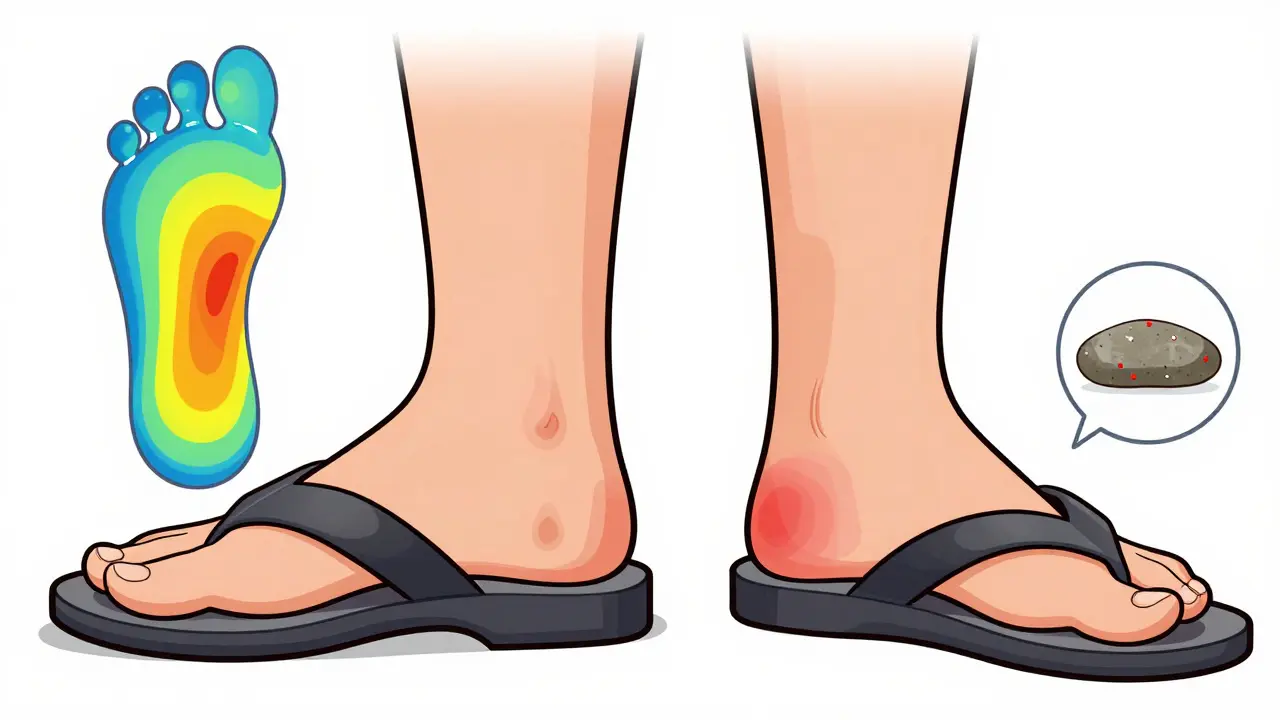
Diabetic foot ulcers don’t appear out of nowhere. They grow from unnoticed injuries. Nerve damage from high blood sugar makes your feet numb. You might step on a pebble, rub your toe against a seam in your shoe, or burn your foot on a hot floor-and feel nothing. By the time you see the problem, it’s already infected. That’s why daily inspection isn’t just a suggestion. It’s your first line of defense.
The Daily Foot Inspection Checklist
Here’s exactly what to do every single day, no exceptions:
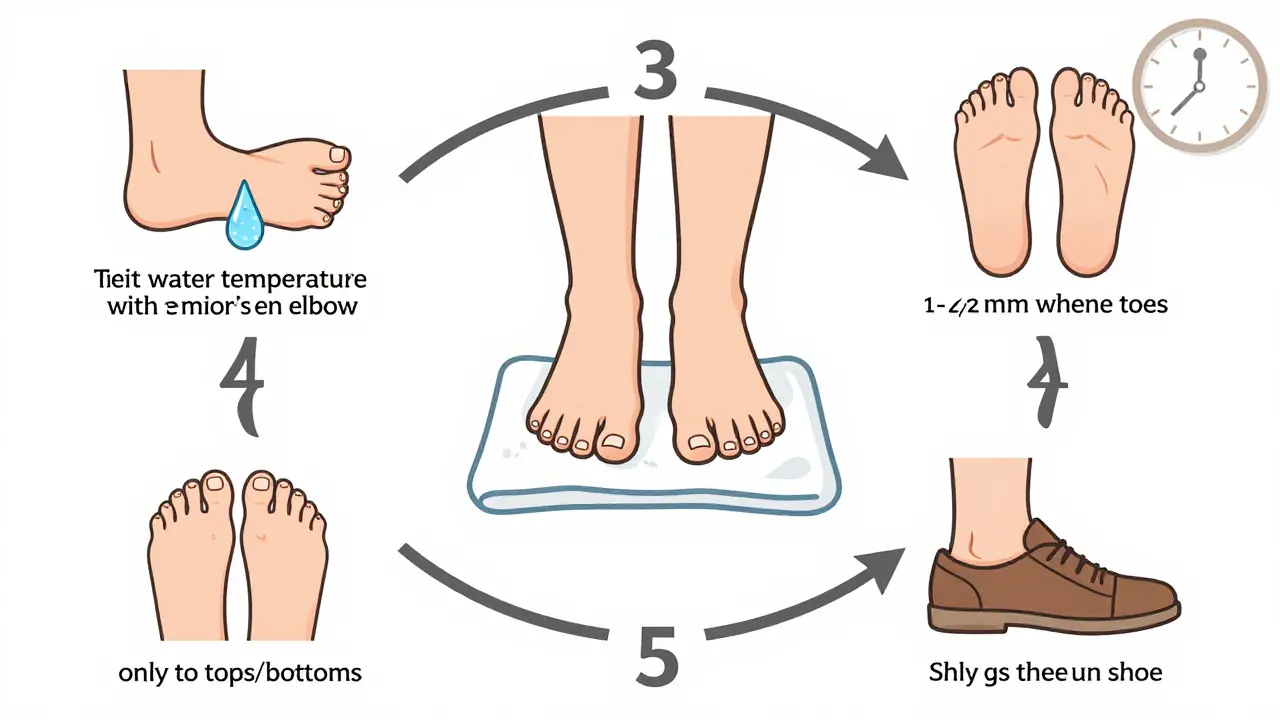
- Wash your feet in lukewarm water (90-95°F). Test the temperature with your elbow or a thermometer. Hot water can burn you without you knowing.
- Dry thoroughly, especially between your toes. Moisture there invites fungal infections and cracks that turn into open sores.
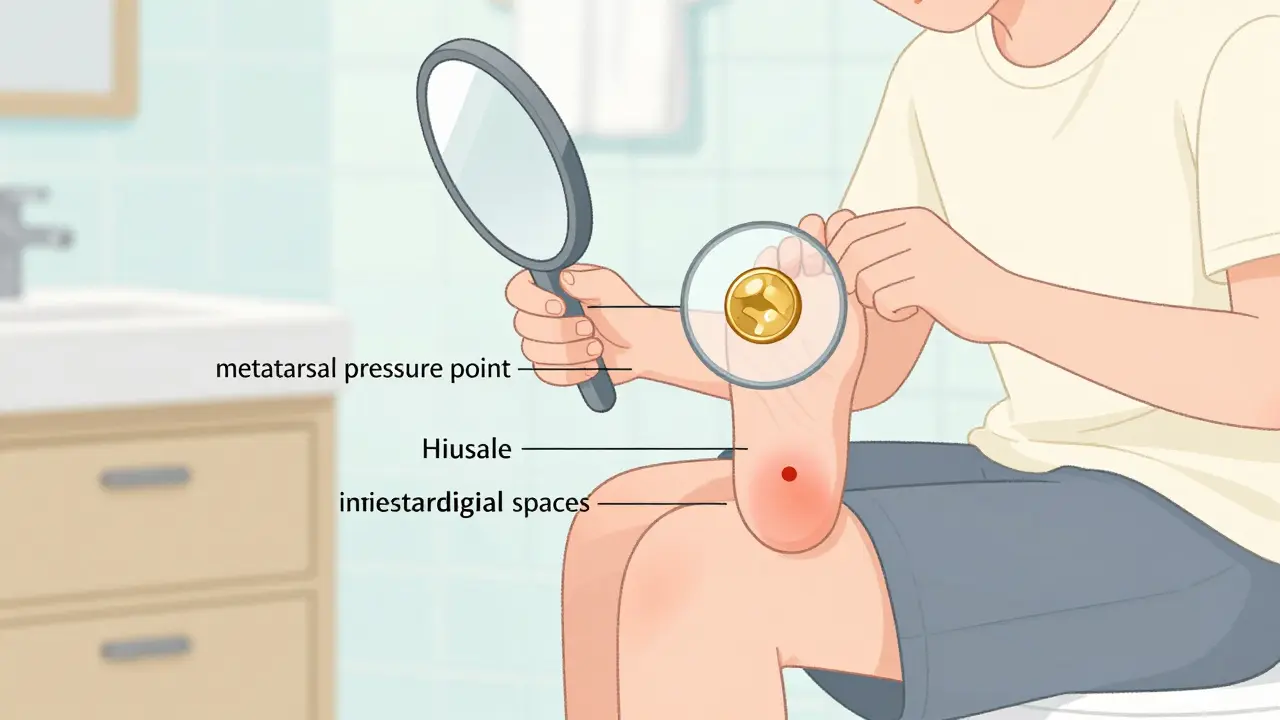
- Inspect every surface using a mirror or ask someone to help. Look at the soles, heels, between toes, and under toenails. Don’t guess-look closely.
- Look for these warning signs: blisters larger than a pea, cuts deeper than a scratch, redness bigger than a coin, swelling that makes your shoe feel tighter, or skin that feels warmer than the other foot.
- Apply moisturizer to dry skin, but never between your toes. Dry skin cracks. Cracks get infected.
- Trim toenails straight across, leaving a sliver of white-about 1-2mm. Don’t round the edges. Ingrown nails are a major cause of ulcers.
- Check your shoes before putting them on. Shake them out. Look for pebbles, torn linings, or sharp seams. One small object can cause a wound you won’t feel.
Do this at the same time every day-ideally between 10 a.m. and 2 p.m. When your body temperature is stable, it’s easier to spot unusual warmth, which is often the first sign of infection.
What Your Feet Are Telling You
Not every red spot is serious. But some changes mean you need to act fast:
- Redness over 1 cm that doesn’t fade after a few hours? That’s inflammation.
- Swelling that increases by 5% or more compared to your other foot? Fluid buildup means something’s wrong.
- Warmth above 99°F on one spot? That’s a red flag for infection. Use a non-contact thermometer if you have one.
- Drainage, odor, or black tissue? Don’t wait. Call your doctor immediately.
Most ulcers start under the ball of the foot-right where your metatarsal bones press down. That’s the spot to check twice as hard. If you’ve had an ulcer before, your risk is even higher. This isn’t a one-time fix. It’s a daily habit.
Footwear That Saves Feet
Shoes aren’t just about comfort-they’re medical equipment for people with diabetes. The wrong pair can cause 87% of forefoot ulcers.
Here’s what to look for:
- Space: At least 0.5 inches (12.7 mm) between your longest toe and the end of the shoe. Your toes need room to move.
- Width: Your foot should sit comfortably without squeezing. Your toes should spread naturally-no pinching.
- Heel support: The back of the shoe should hold your heel firmly without slipping. A rigid heel counter reduces pressure on the midfoot.
- No barefoot walking: Not even in the house. The CDC says walking barefoot increases ulcer risk by more than 11 times-even for just five minutes.
Therapeutic shoes aren’t optional for high-risk patients. If you have nerve damage, foot deformities, or a past ulcer, your doctor should prescribe them. Insurance often covers them. Ask. Don’t assume.
And yes-flip-flops and sandals are risky. They expose your feet to cuts and increase pressure on vulnerable spots. Even in summer, wear closed-toe shoes made for diabetic feet.
When to See a Doctor
You don’t need to wait for an emergency. Schedule regular checkups based on your risk level:
- Risk 0 (no numbness, no past ulcers): Once a year.
- Risk 1 (numbness but no deformity): Every six months.
- Risk 2 (numbness + foot shape changes): Every 3-4 months.
- Risk 3 (past ulcer or amputation): Every month or as directed.
Your doctor should check your sensation with a 10-gram monofilament and your circulation with an ankle-brachial index (ABI) test. If your ABI is below 0.9, you need a vascular specialist. Poor blood flow means even small wounds won’t heal.
If you notice any of the warning signs above, don’t wait. Call your podiatrist or diabetes care team within 24 hours. Early treatment cuts healing time in half and reduces amputation risk by up to 80%.
What Doesn’t Work
There are myths out there that can hurt you:
- Antibiotics for prevention: No. Taking antibiotics to prevent infection in an uninfected wound doesn’t help. It increases resistance and does nothing for healing.
- Nerve surgery: Cutting nerves to relieve pressure doesn’t prevent ulcers. Major studies show it’s ineffective.
- Unsupervised exercise: Ankle exercises without gait analysis can increase ulcer risk by 22%. Move your feet, but get professional guidance first.
- Home remedies: Apple cider vinegar, hydrogen peroxide, or iodine on wounds? These can damage tissue. Clean with saline or water only.
Stick to what’s proven: inspection, proper shoes, moisture control, and professional care.
Barriers and How to Overcome Them
Many people struggle to stick with daily foot care. Here’s why-and how to fix it:
- Bad vision? Use a handheld mirror with a long handle or ask a family member to help. Some apps use your phone’s camera to magnify your feet.
- Neuropathy? The worse your nerve damage, the harder it is to remember. Set a daily alarm. Put your inspection checklist on your bathroom mirror.
- Cost? Therapeutic shoes can be expensive. Medicare and many private insurers cover them if your doctor prescribes them. Ask about financial aid programs.
- Summer heat? People swap shoes for sandals. That’s dangerous. Buy diabetic-friendly open-toe shoes with padded soles and heel support. They exist.
- No internet access? High-tech sensors and apps can help-but aren’t required. The checklist above works without any tech.
Adherence drops sharply without support. Find a buddy-a spouse, sibling, or caregiver-to check in with you weekly. Accountability saves feet.
What’s Working Now
Programs that combine podiatry, diabetes education, and regular follow-ups cut ulcers by 35% and amputations by 42%. These aren’t futuristic ideas-they’re happening in clinics right now.
Some states now require annual foot exams for Medicaid patients. Others are testing AI apps that analyze photos of your feet for early signs of damage. These tools help-but they don’t replace daily inspection.
The goal isn’t perfection. It’s consistency. One missed day won’t cause an ulcer. But 10 missed days? That’s how ulcers start.
Your Foot Care Is Your Power
Diabetes doesn’t have to take your feet. You have control. Every day you inspect your feet, wear the right shoes, and speak up about concerns, you’re reducing your risk. It’s not about being perfect. It’s about showing up.
Start today. Use the checklist. Stick with it. Your feet will thank you-for the rest of your life.
How often should I check my feet if I have diabetes?
You should inspect your feet every single day. The frequency of professional exams depends on your risk level: once a year if you have no nerve damage or past ulcers, every six months if you have numbness, and every 3-4 months if you have foot deformities. If you’ve had an ulcer or amputation before, you need monthly checks.
Can I walk barefoot at home?
No. Walking barefoot-even indoors-increases your risk of foot ulcers by more than 11 times. You might not feel a sharp object, a hot floor, or a rough seam in your sock. Always wear shoes or slippers with closed toes and good support, even at home.
What kind of shoes should I wear?
Wear shoes with at least 0.5 inches of space between your longest toe and the tip, enough width for your toes to spread naturally, and a firm heel counter. Avoid flip-flops, sandals without support, and tight or pointed shoes. If you have nerve damage, deformities, or a past ulcer, your doctor should prescribe therapeutic footwear designed to reduce pressure on high-risk areas.
Is it safe to use lotion between my toes?
No. Moisture between your toes creates a damp environment where fungi thrive, leading to infections that can turn into ulcers. Apply moisturizer to the tops and bottoms of your feet, but keep the areas between your toes dry.
Should I trim my own toenails?
Yes-if you can see and reach your toes safely. Trim them straight across, leaving a small white edge (1-2 mm). Don’t cut into the corners. If you have poor vision, thick nails, or circulation problems, ask your podiatrist to trim them for you.
Do I need special socks?
Yes. Choose socks made of moisture-wicking material like cotton or bamboo, with no seams, no elastic tops, and no tight bands that dig in. Avoid socks with holes or those that are too tight around the calf. Socks should protect your feet without restricting circulation.
Can exercise help prevent foot ulcers?
Yes, but only if it’s safe and supervised. Walking is generally safe for people with good sensation and no active wounds. Avoid high-impact activities or unsupervised ankle exercises, which can increase pressure on vulnerable areas. Always wear proper footwear and check your feet before and after exercising.
What should I do if I notice a small cut on my foot?
Clean it gently with water or saline, pat it dry, apply a thin layer of antibiotic ointment if recommended by your doctor, and cover it with a sterile bandage. Check it daily. If it doesn’t improve in 24-48 hours, or if you see redness, swelling, or drainage, call your healthcare provider immediately. Never ignore even a tiny cut.

Radhika M
December 18, 2025 AT 00:48One time I caught a tiny blister under my big toe-no pain, just redness. I called my podiatrist the next day. They treated it before it turned into anything. That’s how you avoid the nightmare.
Philippa Skiadopoulou
December 18, 2025 AT 03:08Pawan Chaudhary
December 18, 2025 AT 03:21Jonathan Morris
December 18, 2025 AT 06:19Linda Caldwell
December 19, 2025 AT 06:49You’re not lazy. You’re just distracted. This is your superpower now. Wear your socks like armor. Inspect like a detective. Own it.
Anna Giakoumakatou
December 20, 2025 AT 08:47CAROL MUTISO
December 20, 2025 AT 21:00It’s not about being perfect. It’s about being present. And honestly? It’s the only time I really stop and feel my body. Weird, right?
Jessica Salgado
December 21, 2025 AT 03:59amanda s
December 22, 2025 AT 20:31Kent Peterson
December 24, 2025 AT 16:49Josh Potter
December 24, 2025 AT 16:55Jane Wei
December 25, 2025 AT 09:10