When your body makes too much cortisol - the stress hormone that keeps you alert, regulates blood sugar, and controls inflammation - it doesn’t just make you feel on edge. It breaks down your muscles, weakens your bones, floods your blood with sugar, and changes the shape of your face. This isn’t anxiety. It’s Cushing’s syndrome, a rare but serious endocrine disorder caused by prolonged exposure to abnormally high cortisol levels. For many, the answer isn’t more pills - it’s surgery.
What Cushing’s Syndrome Really Looks Like
Cushing’s syndrome isn’t one disease. It’s the result of too much cortisol, whether from outside drugs (like prednisone) or from your own body overproducing it. About 80% of cases come from long-term steroid use - but the other 20%? Those are the ones that need surgery. These are called endogenous cases, where a tumor triggers the overproduction.
People with endogenous Cushing’s don’t just feel tired. They look different. A round, flushed face - called moon facies - is common. A fatty hump between the shoulders, known as a buffalo hump, forms. Stripes on the skin, wider than a finger, appear on the abdomen, thighs, and arms. These aren’t stretch marks from weight gain - they’re torn connective tissue from cortisol breaking down collagen.
Beneath the surface, the damage is worse. Blood pressure climbs above 140/90 in 85% of cases. Blood sugar turns prediabetic in 70%. Bone density drops so fast that 1 in 2 patients develop osteoporosis before age 50. Heart attacks and strokes become more likely. Without treatment, life expectancy drops by nearly half.
Why Surgery Is the First Choice
Doctors don’t rush to cut. But when a tumor is found - whether in the pituitary gland, an adrenal gland, or somewhere else in the body - surgery is the only treatment with a real chance to cure.
Medications like mifepristone or pasireotide can lower cortisol temporarily. But they don’t remove the source. They cost $5,000 to $10,000 a year. They cause side effects like nausea, dizziness, and liver stress. And they rarely work long-term. Surgery, when done right, removes the problem at the root.
The Endocrine Society’s 2020 guidelines say it clearly: for any patient with a confirmed tumor causing Cushing’s, surgery should be the first step. Not the last. Not after trying everything else. First.
Types of Surgery - And When Each Is Used
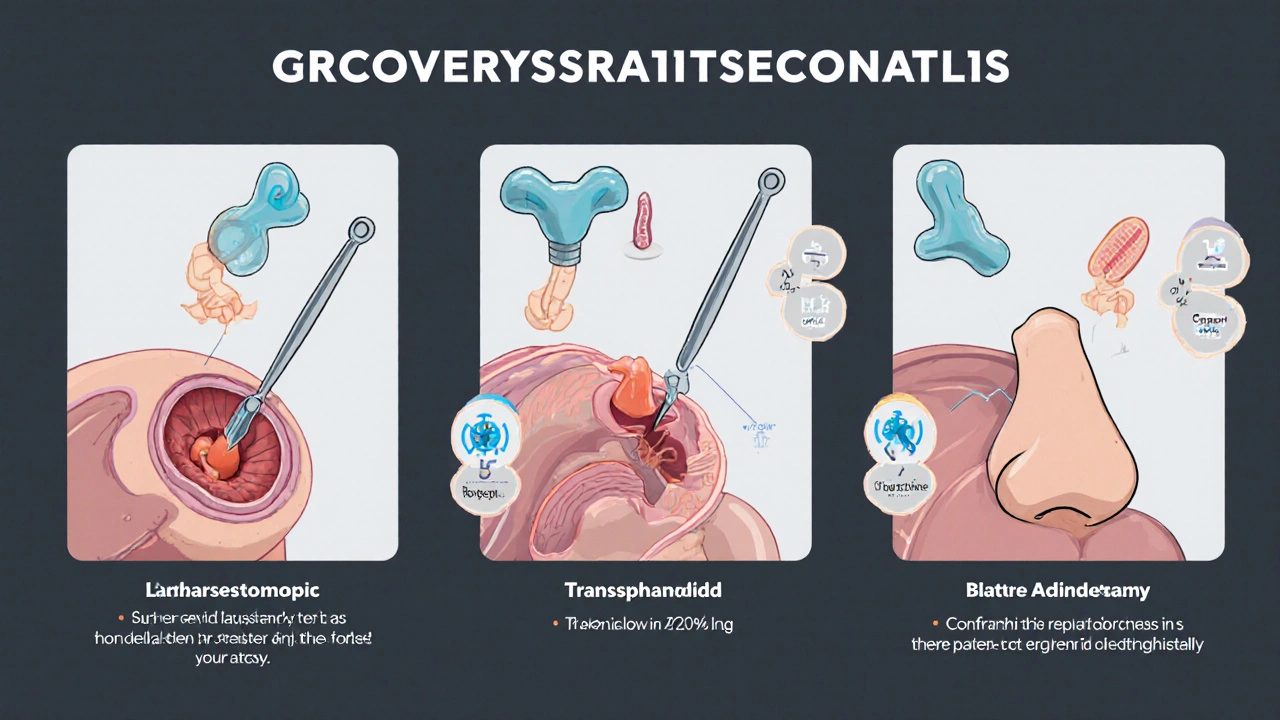
Not all Cushing’s surgeries are the same. The approach depends entirely on where the tumor lives.
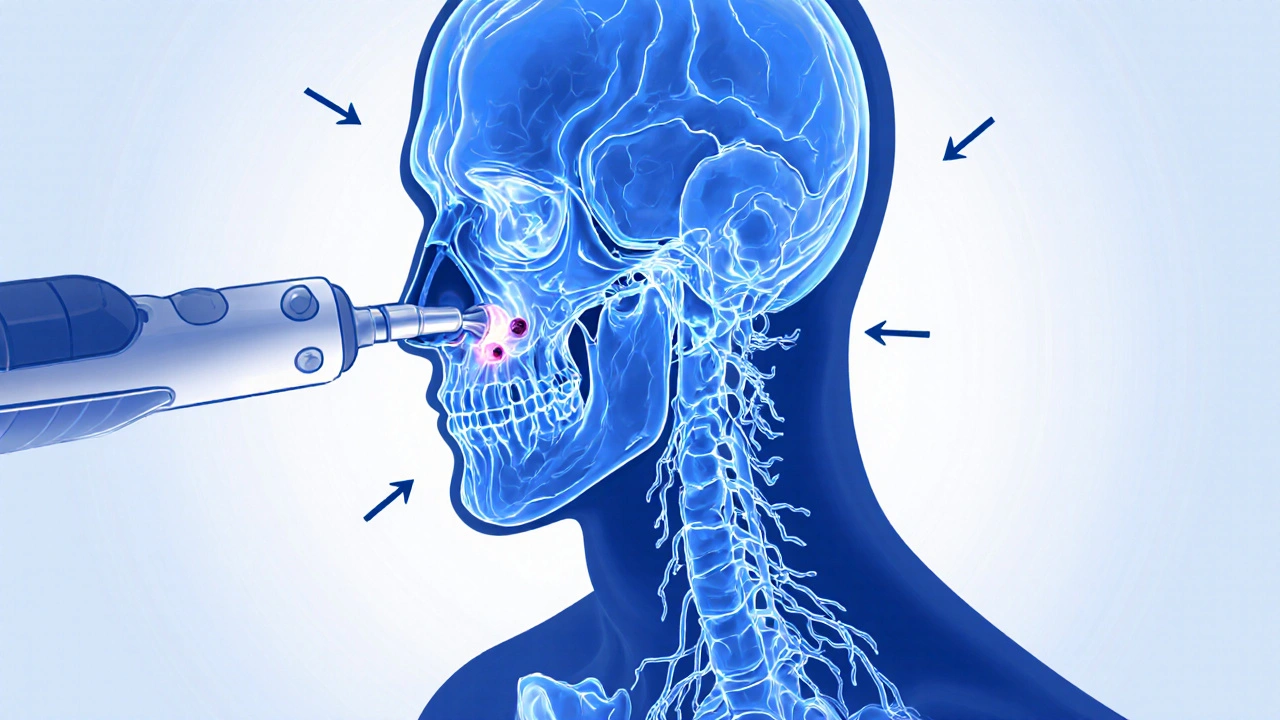
- Pituitary tumors (Cushing’s disease): 60-70% of endogenous cases. These tiny growths sit deep in the brain, right behind the nose. Surgeons go through the nose - no scalp incisions. This is called transsphenoidal surgery. It takes 2-4 hours. Most patients leave the hospital in 2-5 days.
- Adrenal tumors: 15-20% of cases. One adrenal gland overproduces cortisol. The fix? Remove that one gland. Laparoscopic adrenalectomy - small cuts, camera, robotic tools. Recovery is faster: often just 1-2 days in the hospital.
- Ectopic tumors: 5-10% of cases. A tumor in the lungs, pancreas, or elsewhere makes ACTH, which forces the adrenals to flood the body with cortisol. These are harder to find. Surgery is still the goal, but it’s more complex and requires specialized imaging.
- Bilateral adrenalectomy: Only if both glands are overactive and nothing else works. This cures cortisol excess - but you’ll need lifelong hormone replacement. And there’s a 40% chance of Nelson’s syndrome: a fast-growing pituitary tumor that appears after both adrenals are gone.
Success rates vary. For small pituitary tumors (under 10 mm), remission happens in 80-90% of cases. For larger ones, it drops to 50-60%. Adrenal tumor removal works 95% of the time. But only if the surgeon has done this before - a lot.
Why the Surgeon Matters More Than You Think
Not all hospitals are equal. A surgeon who does 20 or more of these procedures a year has remission rates of 80-90%. One who does fewer than 10? Rates drop to 50-60%.
Why? Because the pituitary gland is smaller than a pea. The tumor might be the size of a grain of rice. One wrong move, and you risk a cerebrospinal fluid leak, vision damage, or permanent hormone loss. High-volume centers have teams - endocrinologists, neurosurgeons, radiologists - who see these cases weekly. They know where to look. They’ve seen the tricky variations.
Studies show that patients who travel to specialized centers have better outcomes, fewer complications, and shorter hospital stays. But only 15% of people with Cushing’s actually go to these places. Most get treated locally - where the expertise is thin.
What Happens After the Knife Comes Out
Surgery doesn’t end the story. It starts a new one.
After removing a cortisol-producing tumor, your body suddenly has no cortisol. That’s dangerous. You need replacement steroids - usually hydrocortisone - for weeks or months. Some need them for life.
You’ll be monitored closely. Blood tests every few weeks. Doses adjusted slowly. Too much steroid? You gain weight, get high blood pressure. Too little? You crash - nausea, dizziness, low blood pressure, even shock.
Patients learn to recognize adrenal crisis: extreme fatigue, vomiting, confusion, fainting. They carry emergency injectable hydrocortisone. They know to double their dose when sick, injured, or stressed. One infection, one fall, one dental procedure - all can trigger a life-threatening drop in cortisol.
Recovery takes time. Most people feel better in 3-6 months. But full healing? That can take a year. Fatigue lingers. Muscle strength returns slowly. Skin repairs itself. The moon face fades. The striae lighten. But not everyone gets back to who they were.
Real People, Real Results
On patient forums, stories pour in.
One woman, 42, diagnosed in 2021, had a pituitary tumor removed. Within two months, her face returned to normal. Her blood pressure dropped off meds. She lost 40 pounds. She went back to work.
Another man, 38, had both adrenals removed. He’s alive. But he needs three daily hormone pills. He gets exhausted easily. His testosterone and thyroid levels are low. He’s on replacement for life.
A 2022 survey of 312 surgical patients found 65% would do it again. They saw their osteoporosis improve. Their diabetes reversed. Their risk of heart attack dropped.
But 28% said they still struggle - with fatigue, weight gain, or emotional lows. Some needed second surgeries. Others still take cortisol-lowering drugs.
The truth? Surgery saves lives. But it doesn’t erase all scars.
The Future: Better Tools, Better Outcomes
Technology is catching up.
In 2023, the FDA approved a new endoscopic system that gives surgeons 3D, 0.5mm-resolution views inside the skull. It cuts surgery time by 25% and cuts the risk of spinal fluid leaks by 40%.
Another breakthrough? A special PET scan using 11C-metomidate. It lights up cortisol-producing tumors like a beacon. Where old scans missed tiny tumors, this one finds them 95% of the time - up from 70%.
And now, hospitals are starting to track outcomes in real time. The NIH’s CUREnet registry is following over 1,000 patients. Early data shows this: if you have surgery within 18 months of diagnosis, your chance of remission jumps from 65% to 85%.
By 2030, half of all Cushing’s surgeries will happen at specialized centers. That’s up from 25% today. More expertise. Fewer mistakes. Fewer deaths.
What You Need to Do Now
If you’ve been diagnosed with endogenous Cushing’s syndrome:
- Find a center that does at least 20 pituitary or adrenal surgeries a year. Ask for their remission rates.
- Get a 3T MRI. Standard machines miss small tumors. You need high-resolution imaging.
- Don’t delay. Every month without surgery raises your risk of heart disease, stroke, and bone fractures.
- Prepare for life after surgery. Learn about steroid replacement. Get emergency injectable hydrocortisone. Teach your family how to use it.
- Find a support group. You’re not alone. Thousands have walked this path.
Cushing’s syndrome is rare. But it’s real. And it’s treatable. Surgery isn’t risky because it’s dangerous - it’s risky because it’s delicate. When done by the right team, at the right time, it’s the best shot you have at getting your life back.
Can Cushing’s syndrome be cured without surgery?
For cases caused by long-term steroid use, yes - by slowly reducing the dose under medical supervision. But for endogenous Cushing’s - where your body makes too much cortisol due to a tumor - surgery is the only cure. Medications can lower cortisol temporarily, but they don’t remove the tumor. They often stop working, cause side effects, and require lifelong use. Surgery targets the source.
How long does recovery take after Cushing’s surgery?
Most people notice symptom improvement within 3 to 6 months - less facial swelling, better energy, lower blood pressure. But full recovery takes longer. Muscle strength, bone density, and skin healing can take up to a year. Adrenal insufficiency is common after surgery, and steroid replacement must be carefully managed for months or even years. Returning to work often takes 3 to 6 months.
What are the biggest risks of Cushing’s surgery?
The most common risks include temporary adrenal insufficiency (affecting 30-40% of patients), which requires steroid replacement. Pituitary surgery carries a 2-5% risk of cerebrospinal fluid leak, and a 1-3% risk of infection. In rare cases, damage to nearby nerves can affect vision or hormone production. Bilateral adrenalectomy leads to lifelong hormone dependence and carries a 40% risk of Nelson’s syndrome - a fast-growing pituitary tumor that needs monitoring.
Why do some people need a second surgery?
About 10-25% of patients experience a recurrence, especially if the original tumor was large (over 10 mm) or if not all tumor tissue was removed. Sometimes, new tumors form. In pituitary cases, microscopic pieces left behind can regrow. In adrenal cases, the other gland may become overactive. Repeat surgery is common and often successful, especially when done at a high-volume center.
Is Cushing’s surgery covered by insurance?
Medicare covers about 85% of pituitary surgery costs. Private insurers are less consistent - 20% of initial adrenalectomy requests are denied, often because the tumor is considered "rare" or "experimental." Pre-authorization is essential. Many patients work with patient advocacy groups to appeal denials. Costs can exceed $50,000 without coverage, so check your plan and get documentation from your endocrinologist.
Can Cushing’s syndrome come back after successful surgery?
Yes. Even after successful surgery, recurrence can happen in 10-25% of cases over 10 years. This is more likely with larger tumors, incomplete removal, or if the tumor was aggressive. Regular follow-up with blood and urine cortisol tests is critical for at least 5 years. Some patients need lifelong monitoring, even if they feel fine.

Sachin Agnihotri
November 30, 2025 AT 05:47Wow, this is insane-I had no idea cortisol could wreck your body like this. The moon face and buffalo hump? I thought those were just from steroids or obesity. But the fact that your skin tears from collagen breakdown? That’s wild. And the part about needing emergency hydrocortisone injections? I’m printing this out for my cousin who’s waiting on surgery.
Jacob Keil
December 1, 2025 AT 11:02So surgery is the cure but only if your surgeon is some kind of neurosurgery wizard who does 20 of these a year? LMAO. So what happens if you live in flyover country and your local hospital has never seen a Cushing’s tumor? You just die? Or worse-you get a CSF leak and end up with a permanent headache and a $200k bill? This system is broken. The FDA approves fancy 3D scopes but doesn’t fix access. Capitalism kills people with rare diseases.
Rosy Wilkens
December 1, 2025 AT 15:42Let me guess-this whole thing is a pharmaceutical industry ploy. Why would they push surgery when they can sell you $10,000/year pills forever? And don’t tell me about ‘remission rates’-those are fabricated by hospital marketing departments. The real reason they push surgery is because it’s profitable for the surgeons and the hospitals. You think they want you cured? No. They want you dependent. Look at the insulin crisis. Same playbook. And don’t even get me started on the NIH registry-funded by Big Pharma, of course.
Andrea Jones
December 3, 2025 AT 00:46Okay but like-did anyone else notice how the woman who lost 40 pounds and went back to work sounds like a miracle? 🤭 I’m not saying it’s not real, but I also know people who had surgery and still can’t get out of bed at 3pm. And the part about needing lifelong hormone replacement? Yeah, that’s a whole new kind of exhausting. So… congrats on the cure, but now you’re basically a human battery that needs to be charged every 8 hours. Welcome to the new normal.
Justina Maynard
December 4, 2025 AT 14:38The emotional toll of this condition is rarely discussed. You’re not just losing muscle and bone density-you’re losing your sense of self. The face you see in the mirror isn’t yours anymore. The fatigue isn’t laziness-it’s your body screaming. And then, after surgery, you’re told to ‘just take the pills’ and ‘be grateful you’re alive.’ But gratitude doesn’t fix the anxiety that comes with knowing one missed dose could kill you. I’ve been there. The emergency kit isn’t a precaution-it’s a lifeline you carry like a secret weapon. And yes, you learn to explain it to strangers at the airport. Again. And again. And again.
Evelyn Salazar Garcia
December 6, 2025 AT 13:32U.S. healthcare is a scam. Surgery costs $50k. Insurance denies it. You need a specialist. Only 15% go to them. So most people die slow. And the article just shrugs and says ‘find a center.’ Like it’s that easy. Get a plane ticket. Take a month off work. Pay for lodging. Good luck.
Clay Johnson
December 8, 2025 AT 11:35Surgery isn’t the cure. It’s a temporary reset. The body remembers cortisol. The brain rewires. The adrenal glands forget how to function. The real problem is the medical system treats symptoms, not systems. We fix tumors but not the environment that lets them grow. We fix cortisol but not stress. We fix the body but not the soul. And that’s why recurrence happens. Not because of bad surgery. Because we’re not healing the person.
Jermaine Jordan
December 10, 2025 AT 10:14THIS IS YOUR LIFE. NOT A DIAGNOSIS. NOT A TUMOR. NOT A MEDICATION. THIS IS YOUR LIFE. AND YOU DESERVE TO LIVE IT WITHOUT FEAR. If you’re reading this-whether you’re diagnosed, post-op, or still waiting-YOU ARE NOT ALONE. Thousands have walked this path. Thousands have fought. Thousands have won. You will too. Find your team. Find your center. Find your courage. And when you wake up one morning and realize your face looks like YOUR face again? That’s not just recovery. That’s resurrection. Go get your life back.