Constipation isn’t just about not going to the bathroom often-it’s about struggling to pass hard, dry stools, feeling like you haven’t fully emptied your bowels, or needing to strain for minutes without results. If this happens three or fewer times a week, it’s medically classified as constipation. Around one in three people who visit a doctor for digestive issues are dealing with it. In the U.S. alone, over 2.5 million people seek medical help for constipation every year. It’s not rare. It’s common. And for many, it’s chronic.
Why Does Constipation Happen?
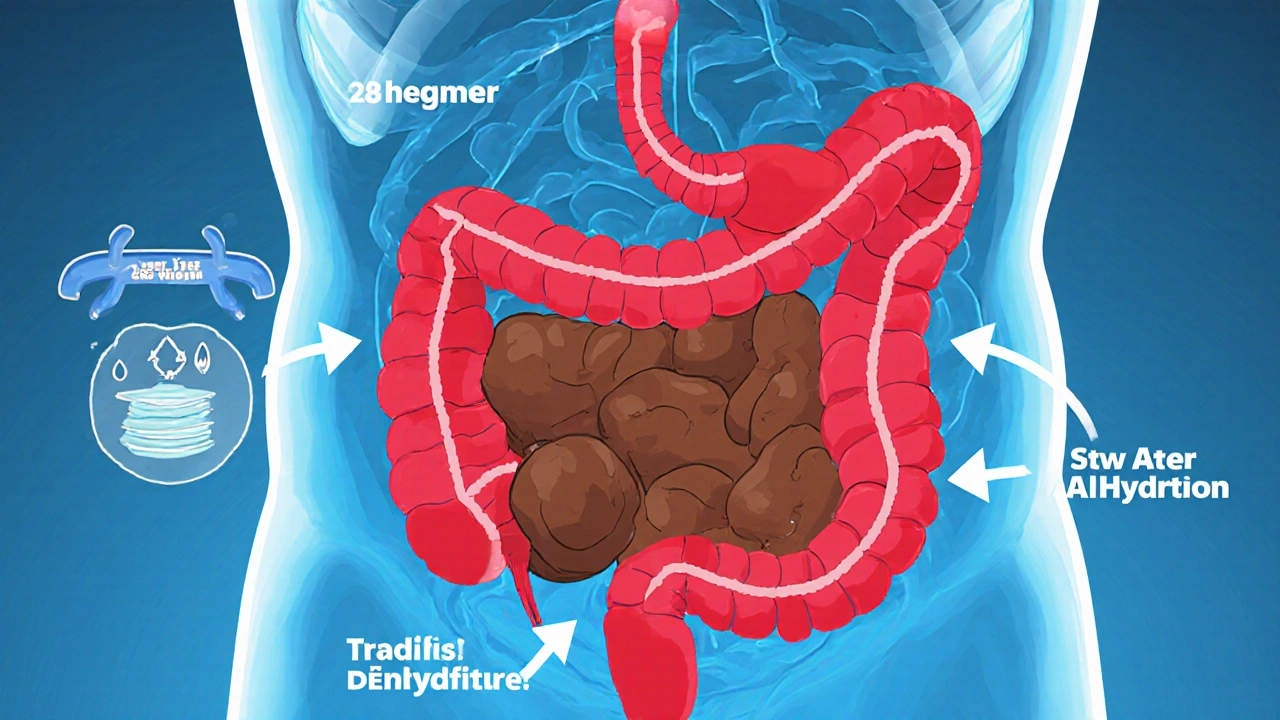
Constipation isn’t one problem-it’s a symptom with many roots. The colon normally moves stool along in 24 to 72 hours. When it slows down, too much water gets pulled out, turning stool into hard, stubborn lumps. But why does that slowdown happen?For most people, it’s lifestyle. Not enough fiber. Not enough water. Sitting too much. The average American eats only 15 grams of fiber a day. Experts recommend 25 to 30 grams. That’s a big gap. Drink less than 1.5 liters of water daily? That makes it worse. Fiber needs water to work. Without it, fiber can actually make constipation worse.
Then there are the hidden causes. Medications are a major one. Opioids-painkillers like oxycodone or morphine-cause constipation in up to 95% of long-term users. Calcium channel blockers for high blood pressure, tricyclic antidepressants, and even iron supplements can slow things down. Diabetes affects nearly 60% of patients with the condition, damaging nerves that control bowel movement. Hypothyroidism, Parkinson’s, multiple sclerosis, and spinal cord injuries all interfere with the signals between brain and gut.
Women are more likely to experience constipation, especially after 60. Hormones, pregnancy, and pelvic floor changes play a role. And it’s not just physical. Stress, ignoring the urge to go, or not having time to sit comfortably on the toilet can train your body to hold it in. Over time, your rectum stops sensing when it’s full.
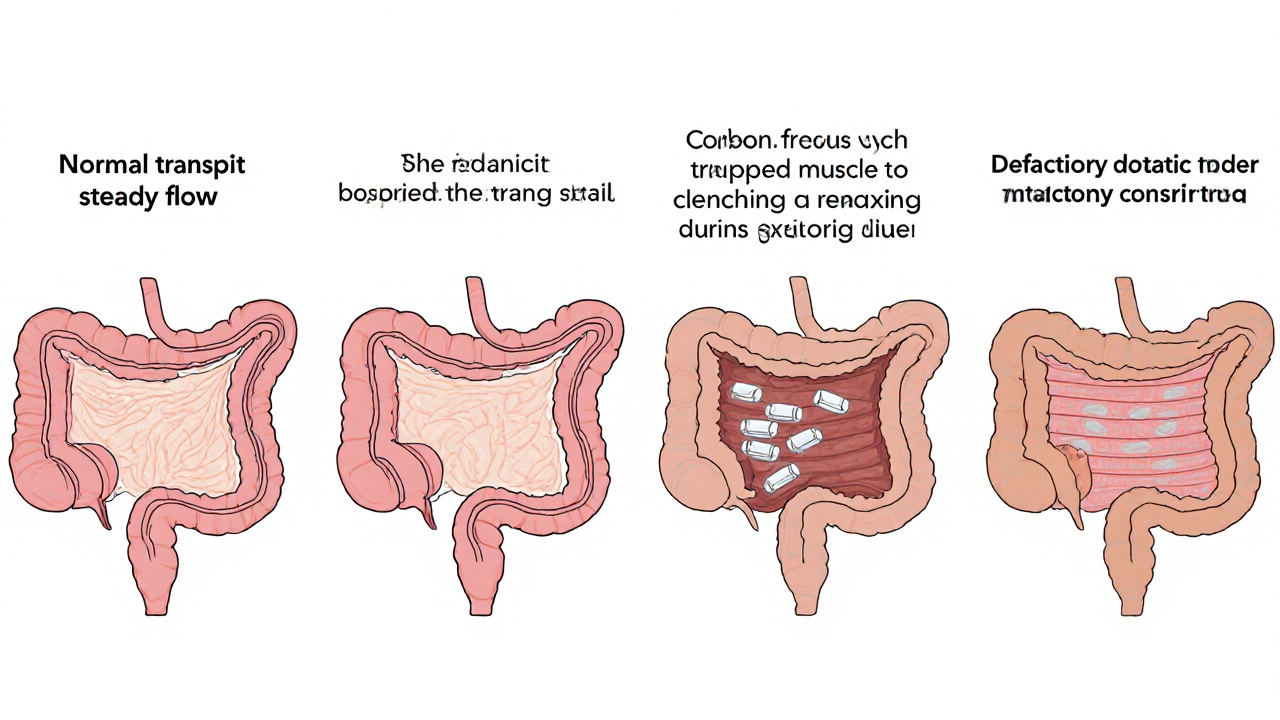
Types of Constipation: Not All Are the Same
There are four main types, and knowing which one you have changes how you treat it.Normal transit constipation is the most common-about 60% of cases. Your colon moves stool at a normal speed, but you still feel straining, hard stools, or incomplete emptying. This often responds well to fiber, fluids, and osmotic laxatives.
Slow transit constipation means stool moves too slowly through the colon-taking more than 72 hours. This is more common in women and older adults. It’s harder to treat with diet alone and often needs stronger medications.
Defecatory disorders affect 20 to 50% of chronic cases. The problem isn’t the colon-it’s the pelvic floor. Muscles that should relax to let stool out instead tighten or don’t coordinate. You might push hard but nothing comes out. This is diagnosed with a balloon expulsion test or anorectal manometry. Biofeedback therapy helps 70 to 80% of people with this issue.
Refractory constipation means symptoms stick around even after trying multiple laxatives. About 15 to 20% of patients fall into this group. These cases often need prescription drugs or even surgery.
Laxatives: What Works and What Doesn’t
Laxatives are the first line of defense-but not all are created equal.Bulk-forming laxatives like psyllium (Metamucil) or methylcellulose (Citrucel) absorb water and swell to form soft, bulky stool. They’re great for normal transit constipation. But here’s the catch: you must drink at least 8 ounces of water with each dose. Without enough fluid, they can cause blockages. About half of users see improvement.
Osmotic laxatives like polyethylene glycol (PEG 3350, Miralax), lactulose, and magnesium hydroxide pull water into the colon. PEG 3350 is the gold standard. It’s effective in 65 to 75% of cases, safe for long-term use, and causes minimal side effects. A daily 17g dose is standard. Unlike stimulants, it doesn’t irritate the colon. This is what most doctors recommend first.
Stimulant laxatives like senna or bisacodyl force the colon to contract. They work fast-often within 6 to 12 hours. But they’re meant for short-term use only. Using them longer than 12 weeks can damage the colon’s natural movement, leading to what’s called cathartic colon. The American Gastroenterological Association warns against using them for more than 3 months.
Stool softeners like docusate sodium are popular but weak. Studies show they’re only 10 to 15% more effective than a placebo. They’re not a standalone solution. Don’t waste money on them unless you’re also using fiber or osmotic laxatives.
For stubborn cases, doctors may prescribe lubiprostone, linaclotide, or plecanatide. These work by activating chloride channels in the gut, pulling fluid into the intestine. Linaclotide helps 45 to 60% of patients with irritable bowel syndrome with constipation. But they’re expensive-over $1,000 a month without insurance.
Long-Term Management: Beyond the Laxative
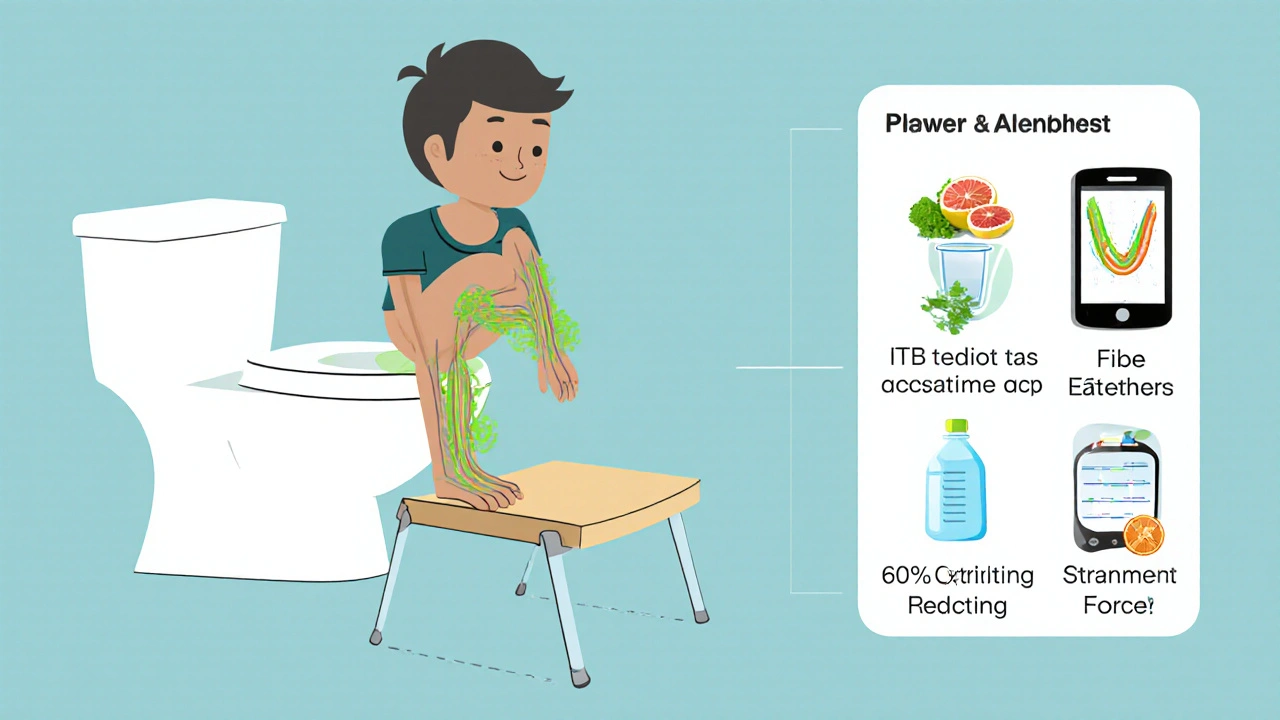
If you’re dealing with constipation for months or years, you need more than pills. Long-term success comes from three pillars: diet, behavior, and body mechanics.Diet is foundational. Don’t suddenly jump from 15g to 30g of fiber. That shocks your gut and causes bloating in 30 to 40% of people. Increase slowly-add 5g every 3 to 4 days. Focus on soluble fiber: oats, beans, apples, pears, chia seeds, and flax. These soften stool better than wheat bran. Drink 1.5 to 2 liters of water daily. Add an extra 250 to 500mL for every 5g of fiber you add.
Behavior matters more than you think. Set aside 10 to 15 minutes after breakfast to sit on the toilet. That’s when your gastrocolic reflex is strongest-the natural urge triggered by eating. Don’t rush. Don’t strain. Read a book. Let your body do the work. If you feel nothing, get up. Trying again later is fine. Forcing it trains your body to ignore signals.
Positioning is a game-changer. Sitting on a standard toilet puts your colon at a 90-degree angle. That’s not ideal. Elevating your feet with a small stool to create a 35-degree hip flexion mimics squatting. Studies show this reduces straining by 60%. It’s simple. It’s free. And it works.
For defecatory disorders, biofeedback therapy is highly effective. A trained therapist uses sensors to show you how your pelvic muscles are working. You learn to relax them when you need to go. Six to eight weekly sessions, each 45 minutes, lead to improvement in 70 to 80% of cases. It’s not cheap-$100 to $150 per session-but it can eliminate the need for laxatives long-term.
When to Worry: Alarm Symptoms
Constipation is usually harmless. But sometimes, it’s a red flag.See a doctor immediately if you have:
- Unintentional weight loss of 10 pounds or more
- Rectal bleeding or dark, tarry stools
- A change in bowel habits lasting more than 6 weeks
- A family history of colorectal cancer
- Severe abdominal pain or vomiting with constipation
These could signal colon cancer, obstruction, or other serious conditions. The American College of Gastroenterology says these symptoms require testing-colonoscopy, blood work, or imaging-not just more laxatives.
Real Stories, Real Results
One woman in her 50s struggled for years. She took senna daily. She felt bloated. She felt dependent. Then she switched: 25g of psyllium husk every morning with 2 liters of water, coffee after breakfast to trigger the reflex, and a footstool every time she sat down. Within 8 weeks, she was going regularly without laxatives. No more anxiety. No more pills.Another man with Parkinson’s had constipation for 12 years. He tried everything. Then his neurologist referred him to biofeedback. After six sessions, he stopped needing laxatives entirely. His quality of life improved more than any medication ever did.
These aren’t outliers. They’re proof that the right approach works-even when meds fail.
What Doesn’t Work (and Why)
Many people believe laxatives are the answer. But relying on them long-term without fixing the root cause is like putting a bandage on a broken bone.Stimulant laxatives become less effective over time. Your colon gets used to them. You need higher doses. Then you get cramps, electrolyte imbalances, or worse. Fiber without water? You get harder stools. Taking magnesium citrate daily? It works-but can cause diarrhea if overdone. And no, prune juice alone won’t fix chronic constipation. It’s a mild aid, not a cure.
Also, don’t assume your doctor knows everything. A Cleveland Clinic survey found 35% of patients received less than 5 minutes of counseling on managing constipation. You need to be your own advocate. Ask about biofeedback. Ask about transit studies. Ask if your meds could be the cause.
What’s New in Constipation Care
Science is catching up. In 2022, the FDA approved tenapanor (Ibsrela) for IBS with constipation. It blocks sodium absorption in the gut, increasing fluid naturally. Early results show 45% of users get adequate relief.Researchers are also studying the gut microbiome. A 2023 NIH project found that people with constipation often have lower levels of Bacteroides uniformis. Future treatments might involve targeted probiotics or prebiotics.
And then there’s AI. Dr. Satish Rao’s team at Augusta University built a smartphone app that analyzes how you push during bowel movements. It detects pelvic floor dysfunction with 85% accuracy. No expensive machines. Just your phone.
The message? Constipation isn’t something you just live with. It’s treatable. But only if you treat the cause-not just the symptom.
How long does it take for fiber to work for constipation?
It usually takes 2 to 4 weeks of consistent fiber intake to see regular improvement. Start with 5g extra per day and increase slowly. If you add too much too fast, you’ll get bloating or gas. Patience is key-fiber works best when combined with plenty of water and time.
Can laxatives cause dependency?
Stimulant laxatives like senna and bisacodyl can lead to dependency if used for more than 3 months. Your colon may lose its natural ability to contract without them. Osmotic laxatives like PEG 3350 don’t cause dependency. They work by drawing water into the colon, not by forcing contractions. They’re safe for long-term use under medical guidance.
Is constipation more common in women?
Yes. About 67% of constipation patients are women. Hormonal shifts during menstruation, pregnancy, and menopause affect gut motility. Pelvic floor changes after childbirth also play a role. Women are more likely to develop defecatory disorders and are often misdiagnosed as having IBS when the real issue is pelvic floor dysfunction.
Should I use enemas or suppositories for chronic constipation?
Enemas and suppositories are for occasional relief, not long-term management. They work quickly but don’t fix the underlying problem. Relying on them regularly can irritate the rectum and lead to dependence. They’re useful for acute blockages or before medical procedures, but not as part of daily routine.
What’s the best way to prevent constipation?
The best prevention is daily habits: eat 25-30g of fiber, drink 1.5-2L of water, move your body (even walking 20 minutes helps), and sit on the toilet after meals without rushing. Use a footstool. Don’t ignore the urge. And if you’re on medications that cause constipation, talk to your doctor about alternatives or protective strategies.

Leo Adi
November 27, 2025 AT 09:34Been dealing with this since my 40s. Switched to psyllium + 3L water daily. No more Miralax. My gut thanked me. Also, footstool changed everything. No joke.
Jauregui Goudy
November 27, 2025 AT 11:12Bro, I was on senna for 5 years. Felt like my colon was a deflated balloon. Started PEG 3350 + fiber + squatting posture. Within 6 weeks, I was regular without anything. No drugs. No guilt. Just science. Seriously, try it. Your body will thank you.
shawn monroe
November 27, 2025 AT 21:58For refractory constipation, lubiprostone is a game-changer if you can afford it. Chloride channel activation > stimulant abuse. Also, don’t sleep on anorectal manometry - if you’re pushing hard and nothing comes out, it’s not ‘just slow transit.’ It’s pelvic floor dyssynergia. Biofeedback is 70-80% effective. Stop treating symptoms. Treat the neuromuscular dysfunction.
Melania Rubio Moreno
November 28, 2025 AT 06:05why do people overcomplicate this? eat more beans drink more water dont sit all day. done. no need for fancy meds or footstools. i just do it.
Gaurav Sharma
November 29, 2025 AT 21:52Let’s be brutally honest: 90% of these ‘lifestyle fixes’ are just lazy people refusing to take responsibility. If your colon is broken, you need a doctor-not a footstool. Biofeedback? That’s for people who can’t handle the truth: you’re addicted to stimulants. Get a colonoscopy. Stop pretending fiber is magic.
Sue Haskett
November 30, 2025 AT 03:33I’ve been a nurse for 22 years. I’ve seen patients on senna for 15 years. I’ve seen them cry because they feel like their body betrayed them. The real tragedy isn’t constipation-it’s that doctors don’t talk about pelvic floor dysfunction. It’s not IBS. It’s not ‘just aging.’ It’s a physical problem with a physical solution. If you’re straining, not emptying, and feeling stuck-ask for manometry. Please.
Lauren Zableckis
December 1, 2025 AT 10:08I used to think this was just a ‘women’s problem.’ Then my dad, 72, got diagnosed with slow transit after being on laxatives since 2010. He started PEG, added chia seeds, and now he walks 30 minutes every morning. He says it’s the first time in decades he’s felt ‘light.’ I’m sharing this because nobody talks about older men with this issue. We need to.
Jebari Lewis
December 2, 2025 AT 05:34As someone who works in GI research, I want to clarify a critical misconception: the term ‘cathartic colon’ is largely outdated. Modern studies show that long-term osmotic laxative use does not cause structural damage to the colon. The real danger is misdiagnosis. Many patients with colonic inertia are mislabeled as having ‘functional constipation’ and are given fiber when they need prokinetics. The data on tenapanor is promising-but access is still a barrier. We need better reimbursement models.
Also, the microbiome angle is fascinating. Bacteroides uniformis depletion correlates strongly with slow transit in longitudinal cohorts. Future probiotics may target this strain specifically. But don’t waste money on generic ‘gut health’ supplements-they’re not standardized.
And yes, the footstool works. A 2021 randomized trial showed a 62% reduction in straining force when using a 15cm stool. It’s not placebo. It’s biomechanics. Your hips are designed to squat. Modern toilets broke that.
Finally, if you’re on opioids, constipation isn’t a side effect-it’s an inevitable consequence. Opioid-induced bowel dysfunction (OIBD) requires prophylactic osmotic agents. Don’t wait until you’re blocked. Start PEG on day one of opioid therapy.
Stop blaming yourself. This isn’t about willpower. It’s about physiology, pharmacology, and poor clinical education.
Asha Jijen
December 3, 2025 AT 12:08lol i tried the footstool and it just made my legs fall asleep. now i just eat prunes and call it a day. why do people make this so hard
archana das
December 5, 2025 AT 03:11Life is like the colon-sometimes you need to slow down, let things soften, and find the right position. Not everything needs to be forced. I used to rush to the bathroom like it was a job interview. Now I sit. I breathe. I wait. And guess what? My body listens. Maybe the answer isn’t more medicine… but more presence.
Edward Batchelder
December 6, 2025 AT 00:18This is why I’m so grateful for people who share real science-not just quick fixes. I’m a caregiver for my mom with Parkinson’s. We tried everything. Then biofeedback. Six sessions. No more suppositories. No more shame. She cried when she realized she didn’t have to live like this. Thank you for writing this. It’s not just medical advice-it’s dignity restored.
Tom Shepherd
December 6, 2025 AT 02:46wait so miralax is safe long term? i thought it was bad. i’ve been taking it for 3 years. i’m kinda freaking out now