When a standard pill just won’t work-because you’re allergic to the dye, can’t swallow tablets, or need a dose that doesn’t exist-compounded medications step in. These aren’t mass-produced drugs from big pharmaceutical companies. They’re made by pharmacists, one at a time, to fit a specific patient’s needs. For some people, they’re the only way to take medicine safely and effectively. But they’re not without risk. Knowing when they’re truly necessary-and when they’re not-can make all the difference in your health.
What Exactly Is a Compounded Medication?
A compounded medication is a custom-made drug created by a pharmacist using raw ingredients to match a prescription that commercial products can’t fulfill. Think of it like baking a cake from scratch instead of buying one pre-made. The pharmacist mixes, measures, and shapes the medicine based on a doctor’s instructions. This could mean changing the strength of a drug, removing an allergen like lactose or gluten, turning a pill into a liquid, or even blending several medications into one capsule.
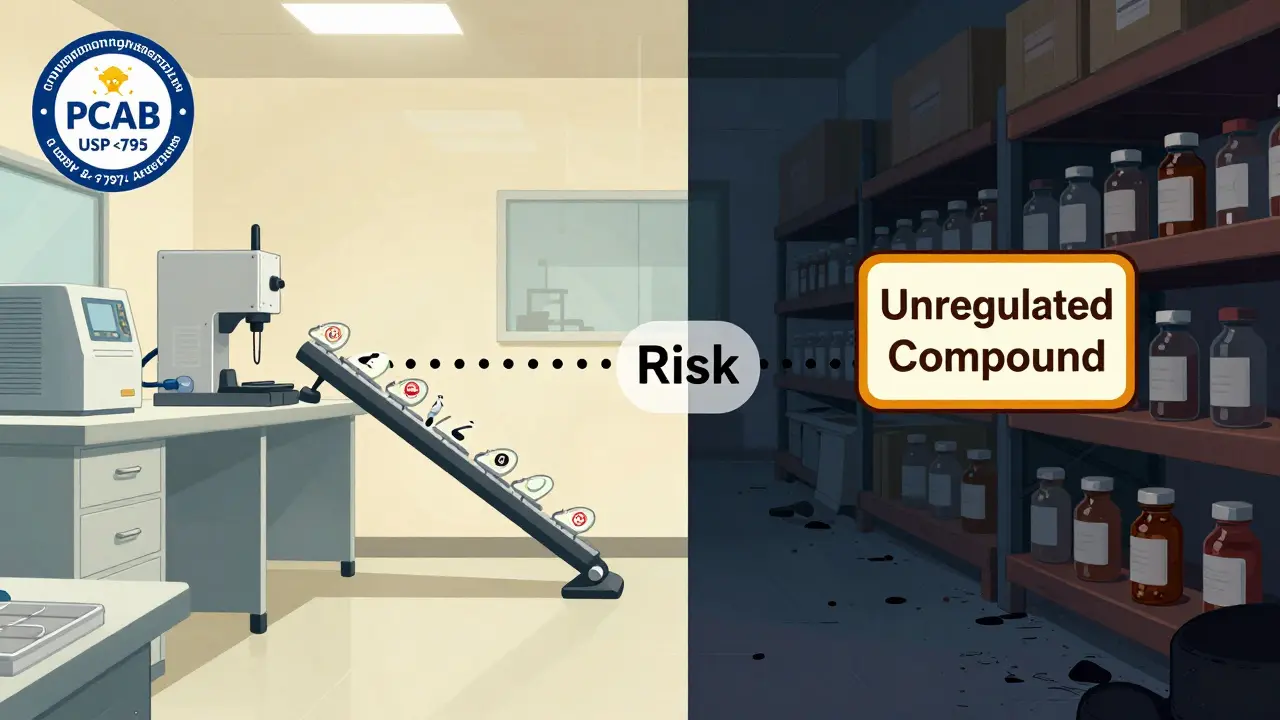
Unlike FDA-approved drugs, compounded medications aren’t tested for safety or effectiveness before they’re given to patients. The FDA doesn’t review them. That’s not because they’re unsafe by design-it’s because they’re made for individuals, not millions. But that also means quality can vary widely depending on the pharmacy.
Why Do People Need Them?
Most prescriptions come in standard doses: 10mg, 25mg, 50mg. But what if you need 12.5mg? Or your child refuses to swallow a pill? Or you’re allergic to the filler in your blood pressure med? That’s where compounding shines.
- Custom dosing: A 65-year-old with kidney issues might need a 0.75mg dose of a medication that’s only sold in 1mg or 2mg tablets. A compounding pharmacist can make exactly what’s needed.
- Allergy-free formulas: About 15 million Americans react to common additives like dyes, preservatives, or lactose. Compounding removes those.
- Alternative forms: If swallowing pills is hard-common in older adults and kids-medications can be turned into creams, gels, lollipops, or liquids. Studies show flavored liquids improve adherence by up to 27% in children.
- Combination drugs: Instead of taking five pills a day, a patient might get one capsule containing all their needed medications. This cuts down on confusion and missed doses.
These aren’t theoretical benefits. Parents of kids with ADHD report adherence jumping from 40% to 95% after switching to a cherry-flavored liquid version. Elderly patients with digestive issues benefit from transdermal gels that deliver medication through the skin instead of the gut.
Where Compounding Falls Short
Compounding isn’t magic. It’s not a replacement for FDA-approved drugs when those drugs are available and safe. And it’s not always reliable.
The 2012 meningitis outbreak linked to contaminated steroid injections from a compounding pharmacy killed 64 people and sickened nearly 800. That tragedy exposed how dangerous poor practices can be. Since then, the FDA has cracked down, but oversight remains uneven.
Compounded medications make up only about 1% of all prescriptions-but they account for 17% of drug recalls between 2010 and 2020. Why? Because unlike factory-made drugs, they don’t go through batch testing, stability studies, or strict quality controls. One batch might be perfect. The next might be too weak-or too strong.
One patient on PatientsLikeMe reported their compounded thyroid medication caused wild swings in their TSH levels. The pharmacist had no way to guarantee consistency between batches. That’s not rare. Without standardized testing, you’re trusting a single pharmacist’s skill and equipment.

Who Should Use Them?
Compounded medications are best suited for specific, well-documented cases:
- Pediatric patients: Kids who can’t swallow pills or need flavors to take medicine.
- Patients with allergies: Those reacting to dyes, gluten, or preservatives in commercial drugs.
- Chronic pain sufferers: Topical creams combining pain relievers, anti-inflammatories, and nerve blockers to avoid systemic side effects.
- Hormone therapy users: Bioidentical hormone formulations tailored to individual levels.
- Veterinary patients: Animals that need tiny doses or unusual forms like flavored treats.
They’re not ideal for:
- Replacing FDA-approved weight loss drugs like semaglutide when those are available and regulated.
- Conditions requiring precise, large-scale dosing (like chemotherapy).
- When a generic version exists and works fine.
Experts agree: compounding should be the exception, not the rule. As Dr. Michael Ganio from ASHP says, “It’s not about convenience. It’s about necessity.”
How to Find a Safe Compounding Pharmacy
Not all compounding pharmacies are equal. There are roughly 7,500 in the U.S. But only about 350 are accredited by the Pharmacy Compounding Accreditation Board (PCAB). That’s less than 5%.
Here’s how to find one you can trust:
- Ask your doctor for a referral. Many know which local pharmacies have strong reputations.
- Check for PCAB accreditation. Visit pcab.org and search their directory. Accredited pharmacies follow strict standards for cleanliness, training, and testing.
- Look for USP compliance. Reputable pharmacies follow USP Chapter <795> for non-sterile compounds and <797> for sterile ones. These cover everything from glove use to air quality.
- Ask about testing. Do they test potency? Purity? Do they use independent labs? If they can’t answer, walk away.
- Check reviews. Specialty compounding pharmacies average 4.6/5 stars on Healthgrades. General pharmacies offering limited compounding? Around 3.8/5.
Don’t be fooled by flashy websites or claims of “bio-identical hormone miracles.” Stick with accredited, transparent pharmacies.
Cost and Insurance: What to Expect
Compounded meds cost more. A simple non-sterile compound might run $30-$100, while a generic version of the same drug could be $10-$50. Sterile injections? $200-$500. That’s because they require specialized equipment, time, and often third-party lab testing.
Insurance coverage is hit or miss. Medicare Part D covers only 42% of compounded claims. Private insurers vary widely. Some won’t cover anything compounded unless it’s deemed medically necessary and no alternative exists. Always check with your insurer before filling a prescription.
Some pharmacies offer cash discounts or payment plans. Ask. Don’t assume it’s unaffordable.
What’s Changing in the Industry?
The FDA is tightening the screws. In 2023, they issued 12 warning letters to compounding pharmacies for issues like improper sterilization and mislabeling. They’re especially focused on pharmacies compounding weight loss drugs like semaglutide in large volumes-essentially acting like drug manufacturers without the oversight.
There’s also exciting innovation. Some pharmacies are starting to use pharmacogenomic testing-analyzing your genes-to tailor medications. One clinic reported 30% better outcomes in patients with CYP2D6 gene variants that affect how their bodies process drugs.
But the big picture hasn’t changed: compounding is a vital tool for a small group of patients who have nowhere else to turn. It’s not a shortcut. It’s a lifeline. And like any lifeline, it needs to be strong, reliable, and properly maintained.
Bottom Line: Use It Wisely
Compounded medications save lives. They let kids take their medicine. They let allergy sufferers get treatment. They let elderly patients avoid pill overload. But they’re not safer just because they’re custom. They’re riskier-because they skip the safety net of FDA approval.
If your doctor suggests a compounded medication, ask:
- Why can’t I use the commercial version?
- Is this pharmacy accredited?
- Will you monitor how I respond?
- What happens if the dose isn’t right?
Don’t be afraid to push back. If the answer is “It’s just easier,” that’s not enough. If the answer is “Your body can’t handle the standard form,” and they point to real evidence-that’s when compounding makes sense.
It’s not about finding the newest, trendiest treatment. It’s about finding the right one-for your body, your needs, and your safety.
Are compounded medications FDA-approved?
No. Compounded medications are not FDA-approved. The FDA does not review them for safety, effectiveness, or quality before they’re given to patients. They’re made under state pharmacy laws, not federal drug manufacturing rules. That’s why it’s critical to use only accredited compounding pharmacies that follow strict standards like USP <795> and <797>.
Can I get compounded medications without a prescription?
No. Federal law requires a valid prescription from a licensed provider-like a doctor, nurse practitioner, or dentist-for any compounded medication. Any pharmacy offering them without a prescription is operating illegally and poses serious safety risks.
How do I know if my compounded medication is working?
Track your symptoms and any side effects. If you’re taking a compounded hormone or pain med, ask your doctor for baseline blood tests or pain assessments before starting. Follow up in 2-4 weeks. If your symptoms don’t improve-or get worse-your dose may be off. Some pharmacies offer batch testing; ask if yours does.
Why are compounded medications so expensive?
They’re made by hand, not in factories. Each batch requires precise measurements, sterile environments (for some), and often third-party lab testing. There’s no bulk discount. A simple cream might cost $50 because it takes 30 minutes of skilled labor and special ingredients. Compare that to a mass-produced pill made for millions-it’s a different process entirely.
Can I switch back to a regular drug later?
Yes-if your situation changes. If you develop tolerance to a compounded cream, or your child learns to swallow pills, or a new FDA-approved version becomes available, talk to your doctor. Compounding isn’t permanent. It’s a bridge to better care when standard options fail.


Siobhan K.
December 22, 2025 AT 02:23Brian Furnell
December 23, 2025 AT 12:26Adrian Thompson
December 24, 2025 AT 07:05Jackie Be
December 25, 2025 AT 16:40John Hay
December 27, 2025 AT 06:04Jon Paramore
December 27, 2025 AT 16:25Teya Derksen Friesen
December 29, 2025 AT 00:09Cara C
December 29, 2025 AT 01:59Erika Putri Aldana
December 29, 2025 AT 22:30Grace Rehman
December 31, 2025 AT 18:32Jerry Peterson
January 2, 2026 AT 00:12