Sedative Combination Risk Calculator
Assess Your Sedative Combination Risk
Enter the sedatives you're currently taking or might be taking. This tool calculates your risk level based on medical evidence about dangerous combinations.
Risk Assessment Result
Select sedatives to see your risk level
Warning: The FDA confirmed in 2016 that combining opioids and benzodiazepines increases fatal overdose risk by 2.5 to 4.5 times. This tool is not medical advice but an educational resource.
Important: Never mix sedatives without consulting your doctor. Even if you've used these combinations before, tolerance doesn't protect you from overdose.
When you take one sedative, your body slows down a little. Take two, and it slows down more. But take three or more? That’s when things turn dangerous - not just risky, but potentially deadly. Mixing sedatives like opioids, benzodiazepines, alcohol, or sleep meds doesn’t just add up. It multiplies. And the result? A dangerous drop in breathing, oxygen levels, and brain function - a cascade that can end in coma or death, even in people who’ve taken these drugs for years without issue.
What Exactly Is CNS Depression?
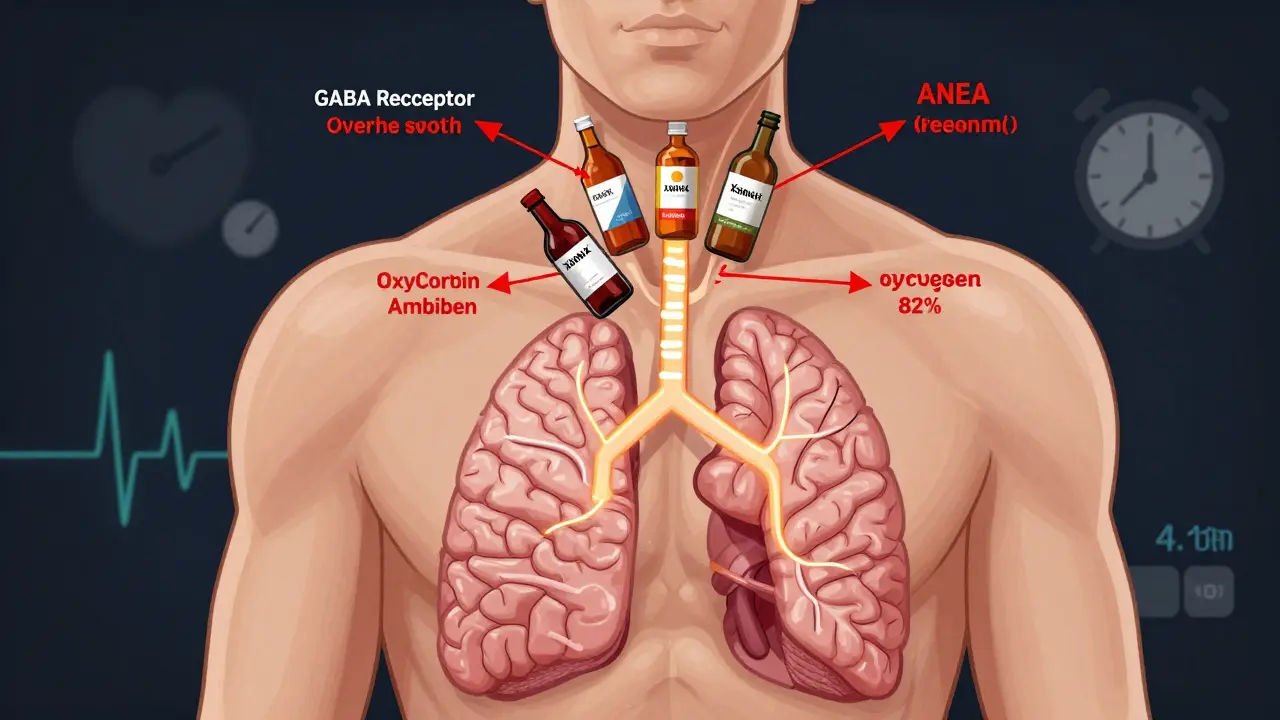
Central nervous system (CNS) depressants are drugs that calm brain activity by boosting a natural chemical called GABA. This slows down signals between your brain and body. Common examples include alprazolam (Xanax), diazepam (Valium), oxycodone (OxyContin), hydrocodone (Vicodin), zolpidem (Ambien), and even alcohol. Individually, they’re prescribed for anxiety, pain, insomnia, or seizures. Together? They can overwhelm your body’s ability to stay alive.
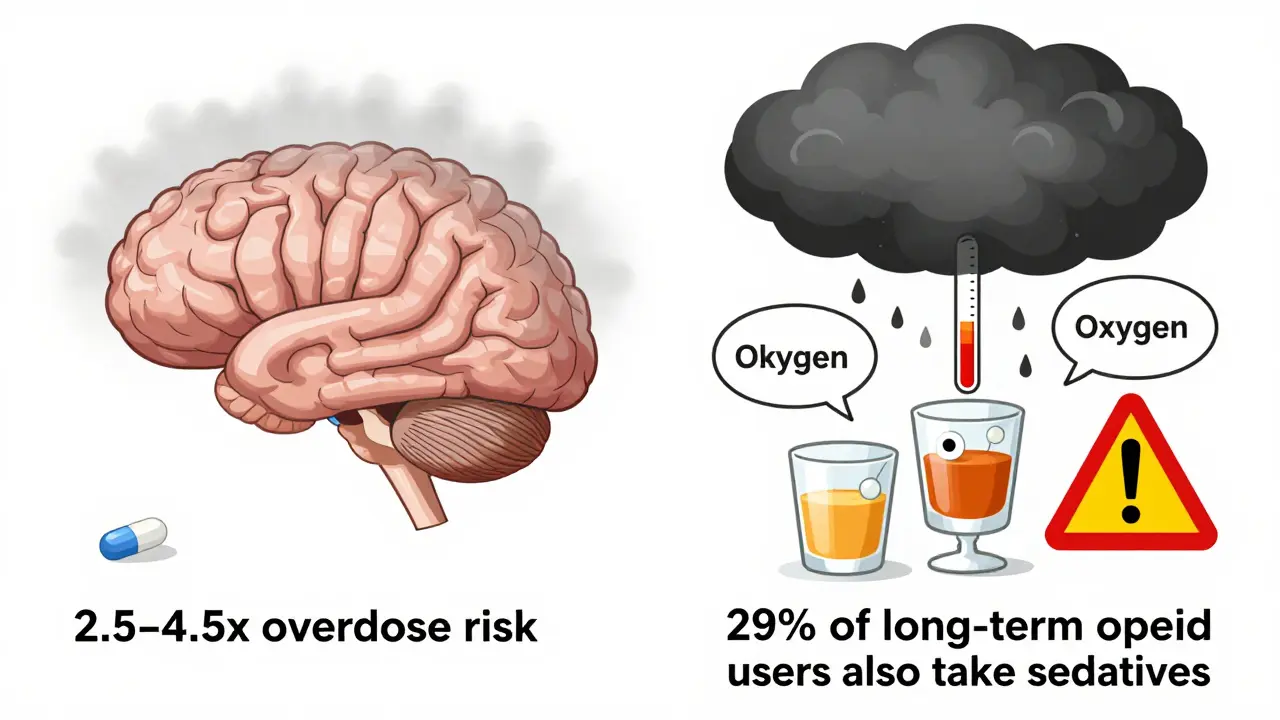
The real danger isn’t just taking two drugs. It’s how they interact. When you combine a benzodiazepine with an opioid, the effect isn’t 1 + 1 = 2. It’s more like 1 + 1 = 4. The FDA confirmed this in 2016, warning that this specific combination increases the risk of fatal overdose by 2.5 to 4.5 times. That’s not a small increase. That’s a life-or-death leap.
The Body’s Breaking Point: What Happens When Sedatives Combine
Your body has limits. When sedatives pile up, your breathing slows - not just a little, but dramatically. Normal breathing is 12 to 20 breaths per minute. When multiple CNS depressants mix, that number can drop to 8, 6, or even 4 breaths per minute. At that point, your lungs aren’t getting enough oxygen. Blood oxygen levels fall below 90%, then below 85%. Within 15 to 20 minutes, your brain starts to suffer.
Here’s what that looks like in real time:
- Confusion or disorientation - reported in 68% of ER visits involving multiple sedatives
- Slowed heart rate - drop of 10 to 20 beats per minute
- Low blood pressure - systolic pressure falls 15 to 25 mmHg
- Dilated pupils, extreme drowsiness, slurred speech
- Loss of consciousness - leading to coma if not treated
After 4 to 6 minutes without enough oxygen, brain cells begin dying. Permanent damage, seizures, or death can follow. And this isn’t rare. A study of 1,848 patients on long-term opioid therapy found that 29% were also taking a sedative - and 12 to 13% were drinking alcohol within two hours of taking their opioid. Many didn’t realize they were putting themselves at risk.
Who’s Most at Risk?
You might think this only happens to people abusing drugs. But the truth is, it’s often people following prescriptions. Elderly patients are especially vulnerable. Their bodies process drugs slower. Their brains are more sensitive. And they’re more likely to be on multiple medications.
Studies show elderly patients taking three or more CNS depressants have a 45% higher risk of being hospitalized after a fall. Why? Because sedatives make you dizzy, unsteady, and slow to react. One study found they were 2.8 times more likely to fall and 3.4 times more likely to break a hip. The American Geriatrics Society lists 34 drugs that should be avoided in older adults - many of them sedatives.
Other high-risk groups:
- People with a history of substance use disorder - 39% use sedatives alongside opioids
- Women - 1.7 times more likely to be prescribed multiple CNS drugs
- Those with depression - 2.1 times more likely to be on a dangerous combo
- Patients on high-dose opioids (100+ morphine milligram equivalents per day)
Even people without addiction can slip into risky patterns. A doctor prescribes Xanax for anxiety. Later, they prescribe OxyContin for back pain. Then, they’re told to take Ambien for sleep. No one connects the dots. And no one warns them: this mix can kill.
Long-Term Damage You Can’t See
The immediate danger gets attention. But the slow, silent damage is just as serious. People who regularly mix sedatives often don’t realize they’re harming themselves over time.
- Chronic fatigue - affects 45% of long-term users
- Weight gain - average of 12 to 18 pounds in a year
- Sleep apnea - develops in 27% of chronic users
- Depression - occurs in 38% of long-term users
- Suicidal thoughts - documented in 19% after just six months
- Cognitive decline - a 5-point drop on memory tests after just months of use
One study tracked elderly patients over time. Those on multiple CNS drugs showed faster mental decline - even after adjusting for age, illness, and other factors. The damage wasn’t sudden. It was steady. And it was preventable.
Why Doctors Still Prescribe Dangerous Combos
You’d think doctors would avoid these combinations. But they often don’t know the full risk. A 2022 study in Frontiers in Psychiatry found that 69% of hospitalizations for major depression involved multiple drugs - yet doctors had almost no clear guidance on which combinations were safe.
Some think: "I’m treating each condition separately. It’s fine." But the body doesn’t work that way. A drug for anxiety doesn’t stay in one system. It affects breathing. A painkiller doesn’t just block pain. It slows your lungs. And when you combine them? The effects don’t cancel out. They amplify.
Even antidepressants can play a role. SSRIs like sertraline or fluoxetine interfere with how the liver breaks down other drugs. That means sedatives build up in the bloodstream - higher than intended. One 2022 study found that combining SSRIs with CNS depressants increased overdose risk by 89% in high-risk patients.
What’s Being Done - And What’s Still Missing
The FDA’s 2016 warning was a turning point. Boxed warnings now appear on opioid and benzodiazepine labels. The CDC recommended against co-prescribing. And between 2014 and 2018, the number of patients getting both dropped by 15.1%.
But progress stalled. In 2020, 10.2% of chronic opioid patients were still getting high-risk benzodiazepine prescriptions. Why? Because prescribing habits change slowly. Because patients don’t always tell doctors about alcohol use. Because electronic systems don’t always flag the danger.
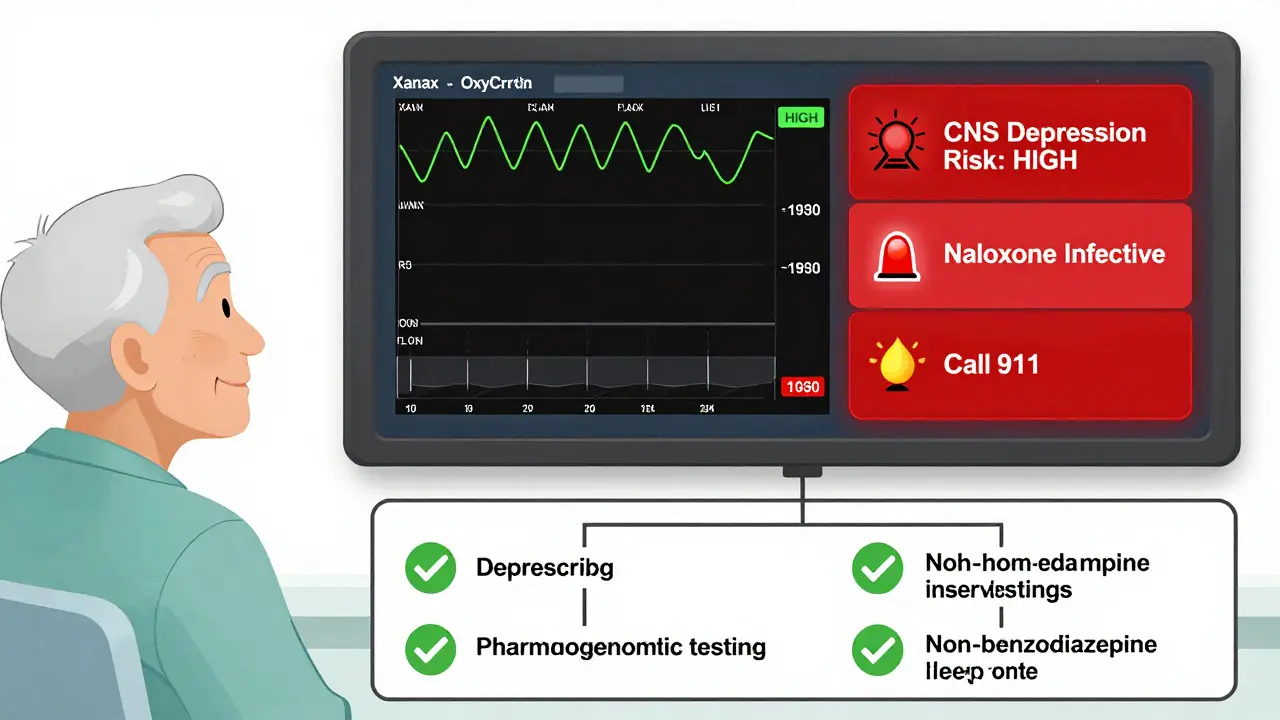
Some hospitals are fixing this. Clinical Decision Support (CDS) systems now automatically warn doctors when a dangerous combo is about to be prescribed. In places where these systems are fully used, inappropriate sedative combinations dropped by 28%.
Other solutions are emerging:
- Deprescribing - slowly reducing or stopping one or more sedatives - reduced falls by 32% and cognitive decline by 27% in one year
- Switching to safer alternatives - replacing long-acting benzodiazepines with non-benzodiazepine sleep aids cut ER visits by 19%
- Pharmacogenomic testing - checking how a person’s genes affect drug metabolism - could reduce dangerous interactions by 22%
- Patient education - teaching people the risks led to a 31% drop in dangerous combinations
By 2025, experts predict all major electronic health records will include mandatory alerts for CNS depressant combos. That could prevent up to 35% of these avoidable deaths.
What You Should Do
If you or someone you know is taking more than one sedative, here’s what to do:
- Review all medications - including over-the-counter sleep aids, alcohol, and herbal supplements. Many people don’t realize melatonin or valerian root can add to CNS depression.
- Ask your doctor - "Is this combination safe? Are there safer alternatives?" Don’t assume it’s fine because it was prescribed.
- Never mix with alcohol - even one drink can push you over the edge.
- Watch for warning signs - excessive drowsiness, confusion, slurred speech, slow breathing, or trouble waking up.
- Carry a medication list - in case of emergency, first responders need to know exactly what’s in your system.
There’s no shame in asking for help. But there’s deadly risk in staying silent.
Can you die from mixing sedatives even if you’ve done it before?
Yes. Tolerance doesn’t protect you from overdose when you combine drugs. What was once a "safe" dose can become deadly when another sedative is added. The body’s response changes with each new interaction. Even if you’ve taken the same mix for years, your metabolism, health, or other medications can shift - making the same dose lethal.
Are over-the-counter sleep aids like melatonin or Benadryl dangerous when mixed with prescription sedatives?
Yes. Melatonin isn’t a strong sedative, but it can add to the effects of other CNS depressants. Benadryl (diphenhydramine) is an antihistamine with strong sedative properties. When combined with opioids or benzodiazepines, it can push breathing rates dangerously low. Many people don’t realize OTC meds count as sedatives - and they’re often the missing piece in a deadly mix.
What should you do if someone passes out after mixing sedatives?
Call 911 immediately. Do not try to wake them by shaking or slapping. Place them on their side to keep their airway open. If you have naloxone (Narcan) and the person took an opioid, administer it. But naloxone won’t reverse the effects of benzodiazepines or alcohol. Emergency medical help is still required. Time matters - brain damage can start within minutes.
Can a doctor legally refuse to prescribe a sedative if I’m already on another one?
Yes. Many doctors now follow CDC and FDA guidelines that strongly discourage co-prescribing opioids and benzodiazepines. Some states have laws requiring prescription drug monitoring before writing new sedative prescriptions. A doctor refusing to prescribe a risky combo isn’t being difficult - they’re following evidence-based safety standards.
Is it safe to stop one sedative cold turkey if I’m mixing them?
No. Stopping benzodiazepines or barbiturates suddenly can cause seizures, extreme anxiety, or even death. If you’re on multiple sedatives, work with your doctor to create a tapering plan. Reducing one drug at a time, under medical supervision, is the only safe way to break the cycle.