When you’re managing asthma, an inhaler with steroids might feel like your lifeline. And for good reason - inhaled corticosteroids (ICS) are the most effective long-term treatment to calm down inflamed airways and prevent flare-ups. But if you’ve been using one for months or years, you might have noticed a scratchy throat, a weird taste in your mouth, or even unexplained bruises. You’re not imagining it. These aren’t rare quirks - they’re real side effects, and they’re completely manageable if you know what to look for and how to act.
What Exactly Are Inhaled Steroids Doing in Your Body?
Inhaled corticosteroids like fluticasone, budesonide, and mometasone work right where you need them: in your lungs. They don’t cure asthma, but they stop the swelling and mucus buildup that triggers wheezing and coughing. Unlike oral steroids that flood your whole body, inhaled versions are designed to stay local. But here’s the catch - no matter how good the design, some of the drug still gets swallowed or absorbed into your bloodstream. That’s where side effects start.
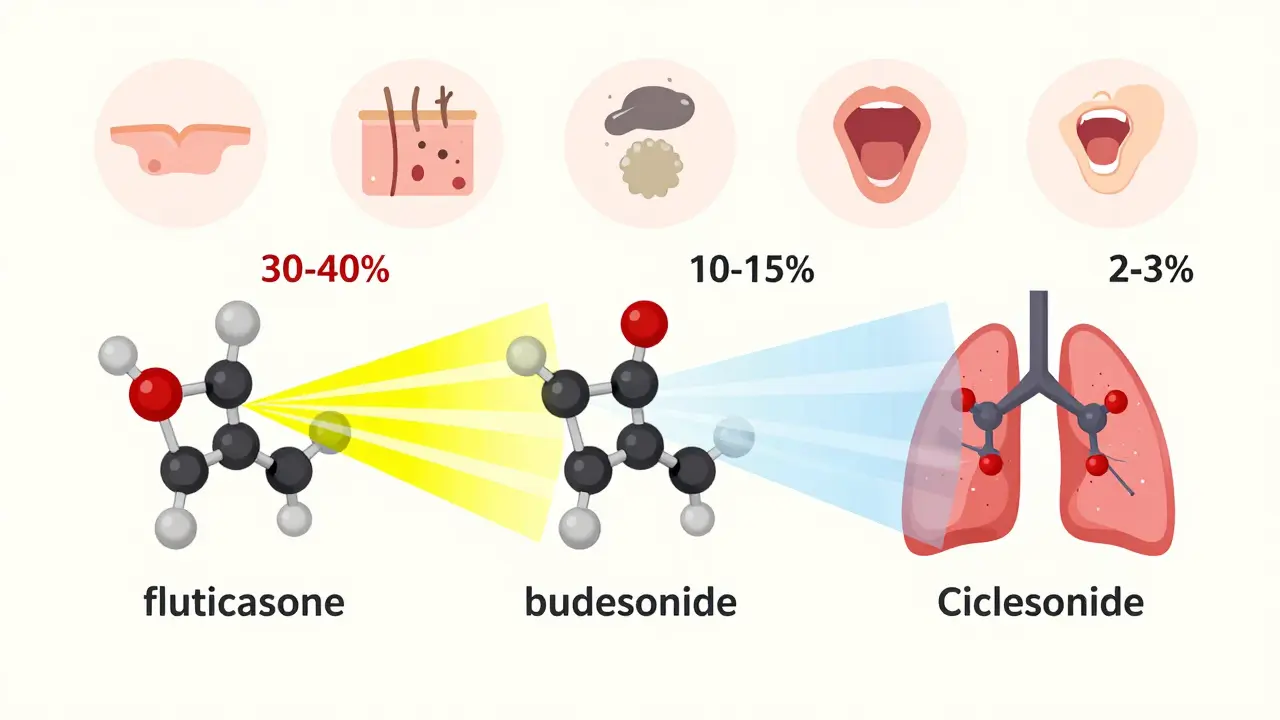
Not all steroids are the same. Fluticasone, for example, gets absorbed into your blood about 30-40% of the time. Budesonide? Only 10-15%. Ciclesonide? As low as 2-3%. That’s not marketing - it’s hard science from clinical trials. And it matters. If you’re on high doses of fluticasone, you’re at higher risk for systemic problems than someone on the same dose of budesonide or ciclesonide.
The Most Common Side Effects (And How to Spot Them Early)
Most side effects from inhaled steroids are local - meaning they happen right in your mouth and throat. These aren’t dangerous, but they’re annoying enough to make people quit their meds. And that’s the real danger.
- Oral thrush - a white, patchy coating on your tongue or inside your cheeks. It’s fungal, not infectious, and it thrives when steroid residue sits in your mouth. One study found 7.3% of fluticasone users got it, but only 4.1% of budesonide users did.
- Hoarse voice or voice changes - often called dysphonia. It’s not permanent, but it can make you sound like you’ve been shouting all day. In surveys, nearly 4 out of 10 users reported this.
- Throat irritation or dry cough - happens when the powder irritates your throat instead of reaching your lungs.
- Skin thinning and easy bruising - especially in older adults. If you notice bruises forming with no memory of bumping into anything, that’s a red flag. People on high doses for over five years had a 34% chance of this - compared to just 5% on low doses.
These aren’t just "side effects" - they’re warning signs. And they’re preventable.
How to Slash Your Risk by 60% (It’s That Simple)
You don’t need to stop your inhaler. You just need to change how you use it.
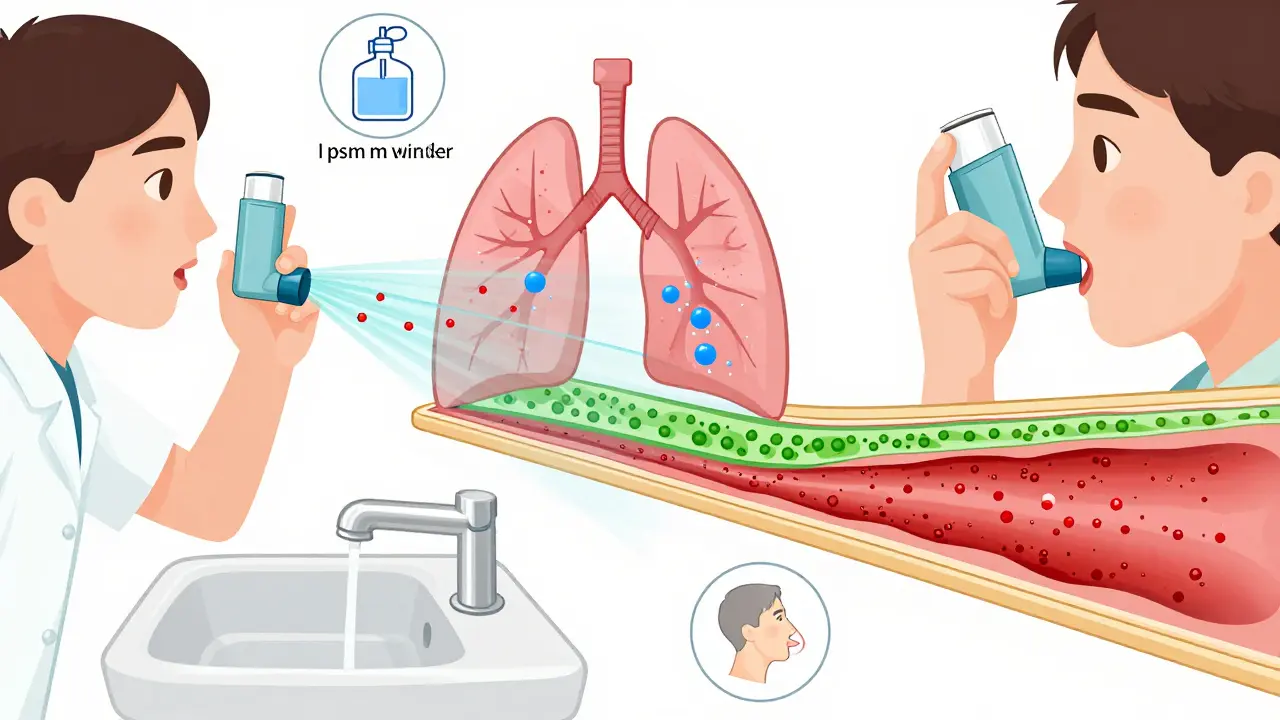
Use a spacer. If you’re using a pressurized inhaler (pMDI), a spacer - that plastic tube you attach to the mouthpiece - is non-negotiable. Without it, only 10-20% of the dose reaches your lungs. The rest sticks to your tongue and throat. With a spacer? That jumps to 60-80%. And your risk of thrush drops by 70-80%. Spacers are cheap, reusable, and covered by most insurance plans.
Rinse and spit - every time. After you inhale, swish water around your mouth for 10 seconds and spit it out. Don’t swallow it. This simple step cuts thrush risk by half. One Cochrane review of 17 studies showed a 57% reduction. That’s not a suggestion - it’s a medical requirement.
Brush your teeth. If you can’t rinse right away, brush your teeth after using your inhaler. It’s not about hygiene - it’s about removing the steroid residue before it sits there all day.
Check your technique. A 2023 study found that 72% of people with side effects had never had their inhaler technique checked by a doctor or nurse. You’d think they’d show you. But only 29% of primary care visits include a technique review. Don’t wait for them to ask. Bring your inhaler to your next appointment and say: "Show me how to use this again."
When Dose Becomes Danger - The Thin Line Between Control and Risk
There’s a sweet spot with inhaled steroids: low enough to avoid side effects, high enough to keep asthma under control. Go above that, and your risk spikes.
Doctors often use a simple rule: 400 mcg/day of beclomethasone is the threshold for minimal systemic risk. That’s roughly 200 mcg/day of fluticasone or 800 mcg/day of budesonide. Above 800 mcg/day, your risk of adrenal suppression - where your body stops making its own cortisol - goes up sharply. That’s not theoretical. In one study, fluticasone at 500 mcg/day was nearly three times more likely to suppress cortisol than budesonide at the same dose.
And it’s not just your hormones. High doses raise your risk of pneumonia - especially if you’re over 65. One study found the chance jumped from 5.2 to 8.9 cases per 100 people each year. That’s a 71% increase. For older adults, that’s not a small risk.
For kids, the concern is growth. At standard doses, ICS may slow growth by less than a centimeter per year - but that adds up. High doses (>800 mcg/day) in children under 12 doubled the risk of cataracts. That’s why pediatric guidelines insist on the lowest effective dose - and regular height tracking.
Who Needs Extra Monitoring?
Not everyone needs the same level of check-ups. But if you fall into one of these groups, ask your doctor about specific screenings:
- Over 65 - annual skin checks for thinning, and bone density scans if you’ve been on high-dose ICS for over five years.
- Pregnant - budesonide is the only ICS with strong safety data during pregnancy. Avoid fluticasone unless absolutely necessary.
- On high doses for over 6 months - ask for a cortisol test if you feel unusually tired, dizzy, or nauseous. A salivary cortisol level below 3 mcg/dL means your adrenal glands are struggling.
- Diabetic - steroids can raise blood sugar. Monitor levels more closely if you’re on high-dose ICS.

The Future: Smarter Inhalers and Steroid-Sparing Treatments
There’s good news on the horizon. Smart inhalers - devices with built-in sensors - now track whether you’re using your inhaler correctly and when you’re using it. One FDA-cleared model detects technique errors with 92% accuracy. That means your doctor can see if you’re skipping rinses or holding your breath wrong - without you having to remember to tell them.
And new drugs are coming. AstraZeneca’s AZD7594, currently in trials, cuts adrenal suppression by 90% compared to fluticasone. It’s not available yet, but it shows where the field is heading: steroids that work like steroids, but act like they’re not steroids.
For people with severe asthma, biologics like dupilumab are already replacing high-dose steroids. In one trial, patients cut their ICS use by 70% and still had fewer attacks. If you’re on high doses and still struggling, ask if you’re a candidate.
Bottom Line: You’re Not Alone - And You Don’t Have to Suffer
Inhaled steroids saved millions from hospitalizations. But they’re not harmless. The key isn’t fear - it’s awareness. You can use them safely if you know how. Use a spacer. Rinse and spit. Ask for a technique check. Keep your dose as low as possible. And don’t ignore those little signs - a hoarse voice, a bruise, a white patch. They’re your body talking.
If you’ve been on an ICS for more than six months, schedule a review. Bring your inhaler. Ask: "Is this the lowest dose I can still control my asthma with?" If your doctor doesn’t ask you about side effects, ask them. Because your safety isn’t an afterthought - it’s part of the treatment.
Do inhaled steroids cause weight gain?
No, inhaled steroids don’t cause weight gain like oral steroids do. Oral steroids flood your system and can increase appetite and fluid retention. Inhaled steroids are designed to stay in your lungs, so systemic effects are minimal - especially at low to moderate doses. Weight gain is rarely linked to ICS unless you’re on very high doses for a long time.
Can I stop using my steroid inhaler if I feel fine?
Don’t stop without talking to your doctor. Even if you feel fine, your airways might still be inflamed. Stopping suddenly can trigger a severe flare-up. Asthma control is like insurance - you don’t notice it working until you need it. Your doctor can help you safely reduce your dose if you’ve been stable for months.
Are there natural alternatives to steroid inhalers?
There are no proven natural replacements for inhaled corticosteroids in controlling persistent asthma. Supplements like vitamin D or omega-3 may support overall lung health, but they don’t reduce airway inflammation like ICS do. For mild asthma, avoiding triggers and using a rescue inhaler may be enough. For moderate to severe asthma, ICS remain the gold standard. Biologics are the only non-steroid medical alternatives - and they’re only for severe cases.
Why does my voice sound different after using my inhaler?
The powder from your inhaler can irritate your vocal cords or coat them with steroid residue, leading to hoarseness - a condition called dysphonia. It’s not permanent, but it’s common. Rinsing your mouth after each use cuts this risk by more than half. If it persists, ask your doctor to check your technique - you might be breathing in too fast or not holding your breath long enough.
How often should I get my inhaler technique checked?
At least every 6 months - or anytime you get a new inhaler, even if it’s the same medication. Studies show that 45-60% of people develop bad habits over time. You might think you’re using it right, but small mistakes - like not shaking the inhaler, or not breathing in slowly - mean you’re getting less medicine and more side effects. Don’t assume you got it right the first time.

brooke wright
January 16, 2026 AT 16:27I used to hate rinsing after my inhaler because it felt like such a hassle. Then I got oral thrush so bad I couldn't eat spicy food for two weeks. Never skipping rinse again. Spacer too. My doctor acted like it was optional. It's not.
Riya Katyal
January 17, 2026 AT 16:38Oh wow, a whole article about not swallowing your medicine? Groundbreaking. I guess the real side effect is trusting doctors who act like inhalers are toothpaste.
Henry Ip
January 18, 2026 AT 13:39This is the most practical asthma advice I've read in years. Spacer + rinse = 80% less junk in your throat. Simple. Cheap. Effective. Why isn't this on every prescription label?
waneta rozwan
January 18, 2026 AT 23:01They say 'low dose' like it's a suggestion. I've been on 1000mcg of fluticasone for 8 years. My skin looks like parchment paper. My bones feel like dry twigs. And my doctor still says 'you're doing great.'
When did 'not dying' become the new baseline for health?
Kasey Summerer
January 19, 2026 AT 09:43Smart inhalers? Cool. Now they'll track how many times I forgot to rinse 😅
Also, I'm pretty sure my dog knows my inhaler routine better than I do.
Samyak Shertok
January 20, 2026 AT 03:56You treat asthma like a machine you can calibrate. But what if your body isn't a machine? What if the inflammation is your soul screaming for stillness? You rinse, you spacer, you track - but do you ever just… breathe? Without fear? Without control?
Or are you just another cog in Big Pharma’s inhaler wheel?
Stephen Tulloch
January 20, 2026 AT 18:21Of course fluticasone is worse than budesonide - it’s basically a steroid slushie for your throat. I switched after my voice sounded like a drunk owl. Now I use ciclesonide. No thrush. No hoarseness. Just peace.
Also, spacers are for people who can’t afford to be lazy. But hey, I’m not judging. 🤷♂️
Melodie Lesesne
January 22, 2026 AT 05:20Thank you for writing this. I was so scared to ask my doctor about my bruising. Now I know it’s not just me aging. And I’m finally getting my technique checked next week. Small wins, right?
swarnima singh
January 23, 2026 AT 11:53they told me i was fine… but my eyes… my eyes have been weird since i started the inhaler… i think they’re watching me… the steroids are in my tears now…
Jody Fahrenkrug
January 25, 2026 AT 02:54I just started using a spacer last month. My throat doesn’t feel like sandpaper anymore. And I didn’t even know I was breathing too fast until someone pointed it out. Thanks for the nudge.
kanchan tiwari
January 26, 2026 AT 17:09They’re hiding the truth. The inhalers are linked to the 5G towers. The white patches? That’s not thrush - it’s electromagnetic residue. They don’t want you to know they’re turning your lungs into WiFi repeaters.
Bobbi-Marie Nova
January 28, 2026 AT 03:18My mom’s been on steroids for 15 years. She still laughs when she says ‘rinse and spit’ like it’s a weird dance move. But she’s alive. And that’s the win.