Warfarin-Amiodarone Interaction Risk Calculator
Important Safety Information
Amiodarone can dramatically increase warfarin effects, leading to dangerous INR levels. This tool provides an estimated risk based on medication doses and is NOT a substitute for medical advice. Always consult your healthcare provider.
Imagine taking three common heart medications - amiodarone, digoxin, and warfarin - because your doctor says they’re necessary. You’re not trying to be risky. You’re just trying to stay alive. But what if these drugs, when taken together, turn into a silent time bomb? This isn’t theoretical. It’s happening in hospitals, clinics, and homes every single day. And too often, it ends in bleeding, hospitalization, or death.
Why This Triad Is So Dangerous
Amiodarone, digoxin, and warfarin are each powerful drugs used to treat heart rhythm problems and prevent blood clots. But when they’re combined, their effects don’t just add up - they multiply. Amiodarone doesn’t just interact with one of them; it hijacks how both digoxin and warfarin work in your body. Digoxin helps control heart rate in atrial fibrillation. But amiodarone blocks the transporter that normally clears digoxin from your blood. That means digoxin builds up. Fast. Within just a few days, your digoxin levels can jump by 70% or more. That’s not a small bump - it’s enough to trigger toxicity. Nausea, vomiting, blurry yellow vision, and dangerous heart rhythms aren’t side effects here - they’re warning signs. At the same time, amiodarone shuts down the liver enzymes (CYP2C9 and CYP3A4) that break down warfarin. Warfarin’s job is to thin your blood. But when it’s not being cleared properly, your INR - the measure of how long it takes your blood to clot - can skyrocket. One study found that 28% of patients on this combo had INRs above 4.0 within two weeks. An INR over 4.0 means your risk of major bleeding jumps dramatically. Over 10? That’s life-threatening. And here’s the kicker: amiodarone sticks around for months after you stop taking it. Its half-life? Up to 100 days. So even if you quit amiodarone, the danger doesn’t disappear. Your warfarin dose still needs to be watched closely for weeks - sometimes two months - after stopping.The Real-World Cost of Overlooking This
This isn’t a rare edge case. The FDA’s Adverse Event Reporting System recorded over 1,800 cases of digoxin toxicity linked to amiodarone between 2010 and 2022. That’s not a typo - 1,800. And the odds of digoxin toxicity are more than five times higher when amiodarone is involved. For warfarin, the numbers are just as scary. One study of nearly 13,000 patients showed that adding amiodarone made it over four times more likely for INR to climb above 4.0. Major bleeding risk went up by 180%. A cardiologist from Massachusetts General Hospital shared a case on Reddit where a patient’s INR hit 12.4 - that’s 12 times the normal clotting time. He needed four units of plasma and a high-dose vitamin K injection just to stop the bleeding. Elderly patients are hit hardest. A 75-year-old with atrial fibrillation, heart failure, and a history of stroke is exactly the kind of person who gets all three drugs. They’re also more likely to fall. And if their blood is too thin? A simple fall can mean a brain bleed. The American Society of Health-System Pharmacists gets an average of 87 calls a month from pharmacists and doctors asking for help managing this exact combo.What Doctors Should Do - And What They Often Don’t
There’s a clear, evidence-based protocol for managing this triad. But too many clinicians still treat it like a routine prescription. When amiodarone is added to a patient already on digoxin and warfarin:- Reduce digoxin by 50% immediately - don’t wait for lab results.
- Check serum digoxin levels 72 hours after starting amiodarone. If it’s above 1.2 ng/mL in someone over 70, you’re already in danger territory.
- Halve the warfarin dose before or at the same time as starting amiodarone.
- Check INR every 48 to 72 hours for the first two weeks. Then weekly for at least four weeks.
- Even after stopping amiodarone, keep checking INR for 4 to 6 weeks. The drug is still in your system.

What Patients Need to Know
If you’re on any of these three drugs - especially two or more - you need to be your own advocate.- Ask your doctor: “Am I on amiodarone, digoxin, and warfarin together? If so, what’s the plan to keep me safe?”
- Know your digoxin level. It should be between 0.5 and 0.9 ng/mL for most people over 70. Anything above 1.2 is a red flag.
- Know your INR. If you’re on warfarin, your target is usually 2.0-3.0. If it goes above 4.0, call your doctor immediately.
- Watch for symptoms: nausea, vomiting, loss of appetite, confusion, yellow-green halos around lights, unusual bruising, nosebleeds, dark stools, or headaches. These aren’t “just side effects.” They’re signs of toxicity or bleeding.
- Don’t skip blood tests. If your doctor says “we’ll check it in a month,” push back. In this combo, a month is too long.
Is There a Safer Alternative?
Yes - and that’s the good news. Newer blood thinners - the DOACs like apixaban, rivaroxaban, and dabigatran - have largely replaced warfarin for most people with atrial fibrillation. They don’t need constant INR checks. And while amiodarone can still affect them slightly (especially dabigatran, which is cleared by P-glycoprotein), the risk of dangerous bleeding is far lower than with warfarin. But here’s the catch: if you have a mechanical heart valve, you still need warfarin. There’s no alternative. That means this dangerous triad isn’t going away. It’s still needed - and still deadly. Also, digoxin is being used less often. Newer drugs like beta-blockers and calcium channel blockers are preferred for rate control. But in older patients with severe heart failure, digoxin still has a role. And when it’s used with amiodarone? The risk stays high.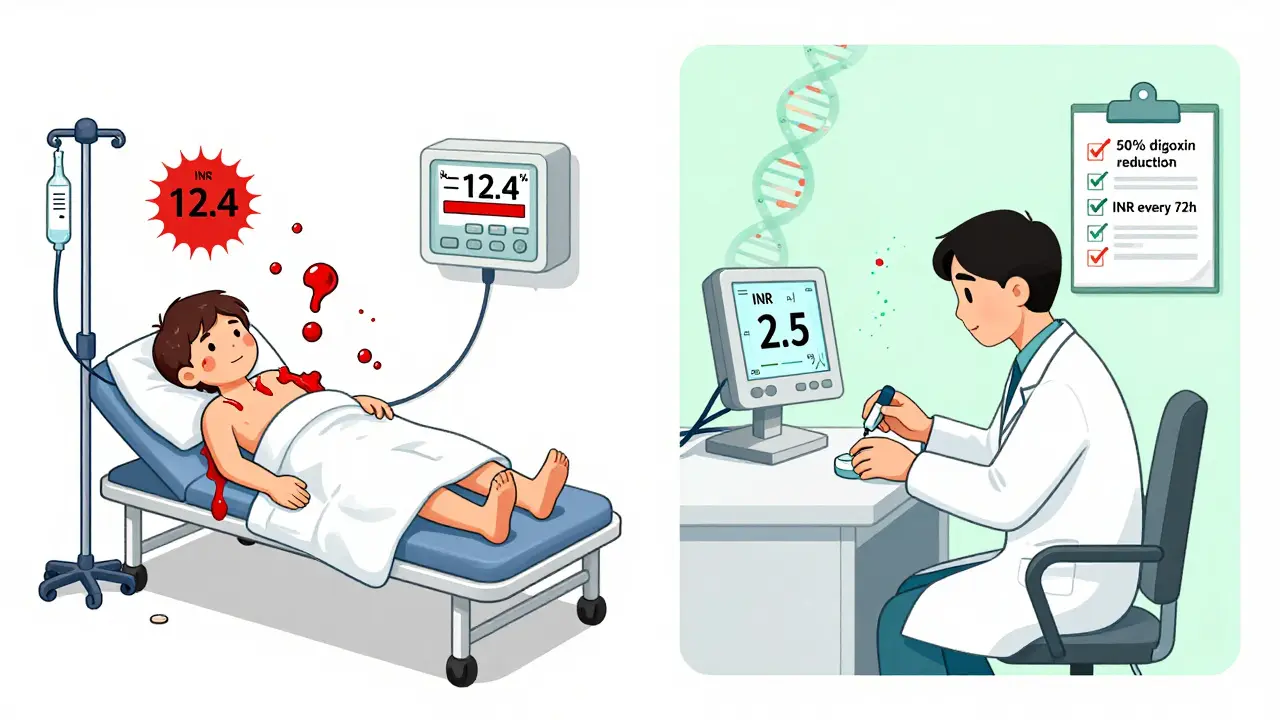
What’s Changing - And What’s Not
Genetic testing is starting to play a role. Some people have a variation in the ABCB1 gene - which controls the P-glycoprotein transporter - that makes them hyper-sensitive to the digoxin-amiodarone interaction. One 2023 study found patients with a certain genetic type had digoxin levels 92% higher than others after starting amiodarone. That’s not just a drug interaction - it’s a genetic time bomb. Electronic health records now have alerts for this combo. One 2022 study showed that hospitals with smart alerts reduced prescribing errors by 65%. But alerts aren’t perfect. If your doctor clicks “ignore,” the system doesn’t stop them. The FDA added a Black Box Warning to amiodarone’s label in 2023 - the strongest warning possible. In 2022 alone, there were 2,147 serious adverse events and 387 deaths tied to this triad. And those numbers are rising.Bottom Line: This Is Not a Minor Interaction
This isn’t about avoiding one extra pill. It’s about understanding that three common, FDA-approved drugs - when taken together - can kill you. The science is clear. The protocols are known. The data is undeniable. The only thing missing is consistent action. If you’re a patient: Ask questions. Know your numbers. Don’t wait for symptoms. If you’re a provider: Don’t assume. Don’t delay. Adjust doses before the problem starts. This triad doesn’t need more research. It needs better practice.Frequently Asked Questions
Can I take amiodarone with digoxin if I’m not on warfarin?
Yes, but it’s still dangerous. Even without warfarin, the amiodarone-digoxin combo increases mortality by 23% according to the 2018 DIG-Amio study. Digoxin levels can spike by 70% or more, leading to toxicity. Dose reduction is still required - usually by 50% - and serum levels must be monitored closely.
How long does it take for amiodarone to affect digoxin and warfarin?
Effects on digoxin can start within 2-7 days. Warfarin’s effect shows up in INR within 3-5 days. But because amiodarone builds up slowly in your tissues, the full impact can take weeks. That’s why monitoring needs to start immediately and continue for months after stopping.
What should I do if my INR suddenly spikes to 6 or higher?
Call your doctor or go to the ER immediately. An INR above 6 puts you at high risk for major bleeding. You may need vitamin K (oral or IV) and possibly fresh frozen plasma. Do not wait for symptoms like bruising or blood in urine. High INR without symptoms is still dangerous.
Can I switch from warfarin to a DOAC to avoid this interaction?
If you have atrial fibrillation without a mechanical heart valve, yes - DOACs like apixaban or rivaroxaban are safer and don’t require frequent blood tests. But if you have a mechanical valve, you must stay on warfarin. Even with DOACs, amiodarone can still raise levels of dabigatran slightly, so caution is still needed.
How often should I get my digoxin level checked after starting amiodarone?
Check it 72 hours after starting amiodarone. Then weekly until stable. After that, check every 2-4 weeks if you’re stable - but if you change doses, get sick, or start a new medication, check it again. Levels above 1.2 ng/mL in older adults are a warning sign.
Why do some doctors still prescribe this combo without adjusting doses?
Many don’t realize how powerful and long-lasting this interaction is. Others assume the patient’s current doses are fine because they’ve been stable. But amiodarone doesn’t work like other drugs - it lingers and builds up. This interaction is under-recognized, especially in older patients who see multiple specialists. Education and electronic alerts help, but they’re not foolproof.


Lu Jelonek
December 25, 2025 AT 08:50I've seen this happen twice in my ICU unit. One patient, 78, on all three meds, ended up with a GI bleed after a minor fall. His INR was 11.2. He didn't even know his digoxin level had been creeping up for weeks. No one checked it after the amiodarone was started. It's not just about dosing - it's about systemic neglect.
Pharmacists are the unsung heroes here. We're the ones catching these before they hit the floor. But we need better communication with prescribers. Not just alerts - actual conversations.
siddharth tiwari
December 26, 2025 AT 12:34govt and big pharma dont want you to know this. amiodarone is a poison they push because its profitable. digoxin is old but safe if used right. warfarin is ancient but works. together? they kill. but why? because they want you dependent. they want you coming back. they want you on more drugs. its all about money. check the patent dates. look at the stock prices. its not medicine. its a business model.
Adarsh Dubey
December 28, 2025 AT 02:39This is one of those cases where the science is rock solid but the practice lags behind. I'm a med student in Delhi and we're taught this interaction in pharmacology class - but in clinical rotations, I've seen it ignored more than once. The issue isn't lack of knowledge. It's time pressure, fragmented care, and the assumption that 'if it's been working, it's fine.'
That mindset kills. This post should be mandatory reading for every resident starting cardiology.
Bartholomew Henry Allen
December 29, 2025 AT 02:21AMERICA IS BEING KILLED BY MEDICAL NEGLIGENCE
DOCTORS AREN'T TRAINED TO THINK
THEY JUST CLICK AND PRESCRIBE
THEY DON'T READ THE LABELS
THEY DON'T CHECK THE LABS
THEY DON'T CARE
THIS IS WHY OUR LIFE EXPECTANCY IS FALLING
THIS IS WHY WE DIE IN OUR 70S
THIS ISN'T A DRUG PROBLEM
IT'S A CULTURE PROBLEM
Dan Gaytan
December 29, 2025 AT 23:21Thank you for posting this. I'm a nurse and I see this all the time. I used to think I was just being paranoid until I saw a patient turn yellow from digoxin toxicity and then bleed out from a warfarin spike. I now print out this exact protocol and hand it to every new attending who prescribes amiodarone. It's not about being pushy - it's about saving lives.
❤️ You're doing the right thing by raising awareness. Keep going.
Delilah Rose
December 30, 2025 AT 17:52It's heartbreaking how many elderly patients are just handed a stack of pills with no real explanation. I had my mom on this combo for six months before I figured out what was going on - she was confused, nauseated, and had these weird yellow rings around her lights. She thought it was just aging. I took her to the ER and the pharmacist there looked at her med list and said, 'Oh god, you're lucky she's still walking.'
It took three weeks of INR checks, a digoxin level adjustment, and a lot of tears to get her stable. I wish I'd known this six months earlier. This isn't just medical jargon - it's a family crisis waiting to happen. Please, if you're reading this and you're on any of these drugs - don't wait for symptoms. Ask now. Ask loudly. Ask again.
Spencer Garcia
January 1, 2026 AT 16:22Halve warfarin at start. Check INR every 48h. Monitor digoxin at 72h. Repeat weekly for 4 weeks. Keep checking for 6 weeks after stopping amiodarone. Done.
Simple. Evidence-based. Life-saving.
Why isn't this in every EHR as a forced alert?
Bret Freeman
January 3, 2026 AT 13:07THIS IS WHY I HATE MODERN MEDICINE
YOU'RE TOLD TO TAKE THREE DRUGS AND THEN LEFT TO DIE
NO ONE TELLS YOU THE TRUTH
THEY SAY 'IT'S FINE' AND THEN YOU'RE IN THE ER
MY UNCLE DIED FROM THIS
HE WAS 72
HE ASKED HIS DOCTOR IF IT WAS SAFE
THE DOCTOR SAID 'YOU'RE FINE'
HE HAD A BRAIN BLEED TWO WEEKS LATER
THE AUTOPSY SAID 'TOXIC DIGOXIN AND WARFARIN'
THEY DIDN'T EVEN CHECK HIS LEVELS
NOBODY CARES
THEY JUST WANT TO GET THROUGH THE APPOINTMENT
THIS IS MURDER BY INDIFFERENCE
Blow Job
January 4, 2026 AT 16:59I'm a pharmacy tech in Ohio. We had a guy come in last month with a 14.7 INR. He was on amiodarone, digoxin, and warfarin. His doctor hadn't adjusted anything. We called the MD - they said, 'Oh, I thought he was off amiodarone.' Turns out he'd been on it for 11 months. We had to rush him to the hospital with vitamin K and plasma. He lived. But he cried in the waiting room because he didn't know he was dying.
Just because you're not bleeding doesn't mean you're safe.
Christine Détraz
January 5, 2026 AT 12:30I'm a 69-year-old on this combo. I was terrified after reading this. I didn't know any of this. My doctor just said, 'You need these to live.' I didn't ask questions because I trusted him. Now I'm checking my INR every week and I asked for a digoxin level - it was 1.3. He lowered my digoxin right away. I'm still scared, but I feel less helpless. If you're on these meds - please, please, please don't stay silent. Ask. Even if you think you're bothering them. You're not. You're saving your own life.
John Pearce CP
January 5, 2026 AT 15:51The systemic failure here is a direct consequence of the erosion of clinical judgment in favor of algorithmic medicine. The reliance on EHR alerts without contextual understanding has created a false sense of security. The fact that 2,147 serious adverse events occurred in 2022 - despite the existence of clear guidelines - is not a failure of pharmacology. It is a failure of governance, education, and professional accountability. The medical establishment must be held to a higher standard than automated pop-ups.
EMMANUEL EMEKAOGBOR
January 6, 2026 AT 07:20I'm from Nigeria and we don't have the resources to check INR or digoxin levels regularly. But we still prescribe these drugs. This post is a wake-up call for low-resource settings too. We need simplified protocols - maybe even a one-page handout for nurses and community pharmacists. Knowledge isn't just power - it's survival. Thank you for making this accessible. We need this translated into Hausa and Yoruba.
CHETAN MANDLECHA
January 6, 2026 AT 11:17Amiodarone is a drug that should be banned from general practice. It's not for primary care. It's for specialists who know what they're doing. Why are family doctors prescribing it? Because they're told to. Because they're pressured. Because they're overworked. This isn't about patient ignorance - it's about system overload. We need fewer drugs, more monitoring, and better training. Not more alerts. More humans.